Dieses Material ist Teil des Leitfadens Pathologiebefund.
- Direkt im Wiki geändert werden sollten Schreibfehler, ergänzende Hinweise.
- Offene Fragen, die der Diskussionen bedürfen, sollten auf der Diskussionsseite aufgenommen werden.
- Liste der Seiten dieses Leitfadens: hier, Liste der Seiten, in denen dieses Material verwendet (transkludiert) siehe hier .
|
Foreword
This is a supplement to the IHE Pathology
and Laboratory Medicine Technical Framework V7.0. Each supplement undergoes a
process of public comment and trial implementation before being incorporated
into the volumes of the Technical Frameworks.
This supplement is published on <Month XX, 2016> for
Public Comment. Comments are invited and may be submitted at http://www.ihe.net/<domain>/<domain>comments.cfm.
In order to be considered in development of the Trial Implementation version of
the supplement, comments must be received by <Month XX, 201X>.
This supplement describes changes to the
existing technical framework documents.
“Boxed” instructions like the sample
below indicate to the Volume Editor how to integrate the relevant section(s)
into the relevant Technical Framework volume.
Replace Section X.X by the following:
Where the amendment adds text, make the added
text bold underline. Where the amendment removes
text, make the removed text bold strikethrough.
When entire new sections are added, introduce with editor’s instructions to
“add new text” or similar, which for readability are not bolded or underlined.
General information about IHE can be found at: http://www.ihe.net.
Information about the IHE Pathology and Laboratory Medicine domain can be found at: http://ihe.net/IHE_Domains.
Information about the structure of IHE Technical Frameworks and Supplements can be found at: http://ihe.net/IHE_Process and http://ihe.net/Profiles.
The current version of the IHE Technical Framework (if applicable) can be found at: http://ihe.net/Technical_Frameworks.
<Comments may be submitted on IHE Technical Framework templates any time at http://ihe.net/ihetemplates.cfm. Please enter comments/issues as soon as they are found. Do not wait until a future review cycle is announced.
Introduction to this Supplement
This supplement complements volume 1 of
the PaLM technical framework with the description of the APSR 2.0 content
profile, and volumes 3 and 4 with the bindings, content modules and value sets, which specify
this profile.
Open Issues and Questions
None yet
Closed Issues
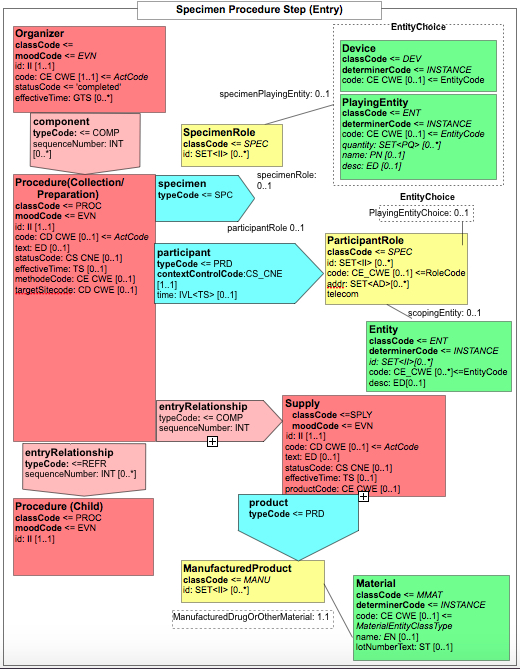
APSR-07 – Representing the hierarchy of specimens in an entry : This APSR
supplement enables to represent the hierarchy of specimens at the CDA level 3.
The operations on specimen and production of child specimens are tracked in the
“Procedure Steps” section, which has a level 3 entry.
APSR-10 – Observation related to multiple specimens: For example tumor staging may require combining data from multiple specimens (e.g., a breast excision with positive margins followed by a re-excision with clear margins – in this case the tumor size may be a composite of measurements from both specimens. Another example is staging of ovarian carcinomas with multiple biopsies of pelvis, peritoneum, nodes, omentum, etc.). To accommodate these use
cases, each problem organizer as well as each observation may reference any number of specimens using the <specimen> child element. Each of these references may point to a detailed description of the specimen, in the "procedure steps" section.
APSR-11 – Derivative specimens:Specimens
derived from primary specimens for ancillary studies, which may be sent to a
reference lab or done in another part of the same institution, are included in
the scope of this profile. The results produced on a derived specimen are
attached to this specimen in the report.
VOLUME 1 - PROFILES
10 Anatomic Pathology Structured Report (APSR) Profile
This content profile describes an
anatomic pathology structured report (APSR) as a digital document to be shared or
exchanged between pathology laboratories and other care providers and
institutions.
Anatomic pathology structured reports
document the findings on specimens removed from patients for diagnostic or
therapeutic reasons. This information can be used for patient care, clinical
research and epidemiology. Standardizing and computerizing anatomic pathology
reports is necessary to improve the quality of reporting and to facilitate the
exchange the exchange and reuse of the content of these reports.
This content profile describes a digital
anatomic pathology report shared in a human-readable format, which may include
images, and which also contains findings and observations in a machine-readable
format, to facilitate the integration of these into the database of a consumer
system, and to enable the application of automated reasoning to this content.
The scope of this IHE content profile covers all fields
of anatomic pathology (cancers, benign neoplasms as well as non-neoplastic
conditions) as well as cytopathology.
Goldsmith, J.D., et al., “Reporting
guidelines for clinical laboratory reports in surgical pathology” Arch Pathol
Lab Med, 2008. 132(10): p. 1608-16, is the first source of specification for
this content profile. This article delineates the required, preferred, and
optional elements which should be included in any report of surgical pathology.
This source is complemented by the
“cancer checklists” produced by the College of American Pathologists, and by
the “comptes rendus d’anatomopathologie : données minimales à renseigner pour
une tumeur primitive” produced by the French society of pathology (SFP [1])
for the French cancer institute (INCa [www.e-cancer.fr]).
This profile has also benefited from the
guidance on cancer AP reports provided by the North-American Association of
Central Cancer Registries; some of the example snippets captured in the profile
leverage the NAACCR Standards for Cancer Registries, Volume V, Pathology
Laboratory Electronic Reporting.
10.1 APSR Actors/Transactions
This
section defines the actors, transactions, and/or content modules in this
profile. General definitions of actors are given in the Technical Frameworks
General Introduction Appendix A published here.
Figure 10.1-1
shows the actors directly involved in the APSR Profile and the direction that
the content is exchanged.
A
product implementation using this profile must group actors from this profile
with actors from a workflow or transport profile to be functional. The grouping
of the content module described in this profile to specific actors is described
in more detail in the “Required Actor Groupings” section below.
Figure 10.1-1 APSR Actor Diagram
Table 10.1-1 lists the content module(s)
defined in the APSR profile. To claim support with this profile, an actor shall
support all required content modules (labeled “R”) and may support optional
content modules (labeled “O”).
Table 10.1-1: <Profile Acronym>Profile - Actors and Content Modules
| Actors |
Content Modules |
Optionality |
Reference
|
| Content
Creator
|
Anatomic Pathology Structured Report
1.3.6.1.4.1.19376.1.8.1.1.1
|
R
|
PaLM TF-3: 6.3.1.2
|
| Content
Consumer
|
Anatomic Pathology Structured Report
1.3.6.1.4.1.19376.1.8.1.1.1
|
R
|
PaLM TF-3: 6.3.1.2
|
10.1.1 Actor Descriptions and Actor Profile Requirements
Most requirements are documented in
Content Modules (Volume 3). This section documents any additional requirements
on profile’s actors.
10.2 APSR Actor Options
Options that may be selected for each
actor in this profile are listed in the table 10.2-1. These options are further
detailed in PCC Technical Framework Volume 2 as indicated in the rightmost
column.
Table 10.2-1 Anatomic Pathology Structured Report - Actors and Options
| Actor |
Option Name |
Reference
|
| Content
Creator
|
None
|
|
| Content
Consumer
|
View Option (1)
Document Import Option (1)
Section Import Option (1)
|
PCC TF-2:3.1.1
PCC TF-2:3.1.2
PCC TF-2:3.1.3
|
Note 1: The Content Consumer Actor shall support at
least one of these options.
10.3 APSR Required Actor Groupings
An Actor from this profile (Column 1)
shall implement all of the required transactions and/or content modules in this
profile in addition to all of the transactions required for the grouped
actor (Column 2).
In some cases, required groupings are
defined as at least one of an enumerated set of possible actors; this is
designated by merging column one into a single cell spanning multiple potential
grouped actors. Notes are used to highlight this situation.
Section 10.5 describes some optional
groupings that may be of interest for security considerations and section 10.6
describes some optional groupings in other related profiles.
Table 10.3-1: Anatomic Pathology Structured Report - Required Actor Groupings
| XD-LAB Actor |
Actor to be grouped with |
Reference |
Content Bindings Reference
|
| Content
Creator
|
ITI XDS.b
Document Source
OR
ITI XDM Portable Media Creator
OR
ITI XDR Document
Source
|
ITI TF-1:10
ITI TF-1:16
ITI TF-1:15
|
|
| Content
Consumer
|
ITI XDS.b Document Consumer
OR
ITI XDM Portable Media Consumer
OR
ITI XDR Document
Recipient
|
ITI TF-1:10
ITI TF-1:16
ITI TF-1:15
|
|
Note 1: Each
actor of APSR SHALL be grouped with at least one of the ITI actors listed in
its table row.
10.4 APSR Overview
10.4.1 Concepts
This content profile represents a common
digital document model applicable to any structured report for surgical
pathology in all fields of anatomic pathology (cancers, benign neoplasms, non-neoplastic
conditions) as well as for cytopathology.
This common model is composed of a header conveying
the context of care (patient, care providers, pathologists, laboratories,
order, act documented …) and a body. The body organizes the human-readable
content of the report in a number of sections. Each section may also provide
machine-readable content in a repeatable “entry” embedded in the section. This common model defines the order of
appearance, cardinalities and internal structure of each section, and of each
entry embedded in each section.
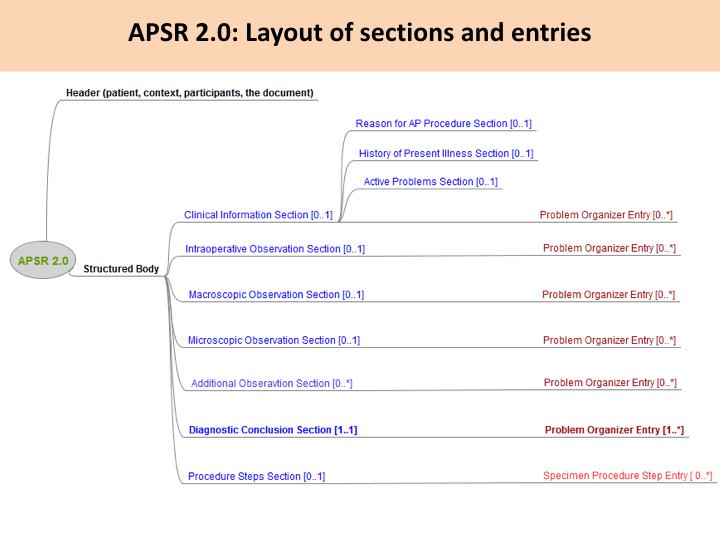
Figure 10.4.1-1 shows this general model
applicable to any pathology digital report.
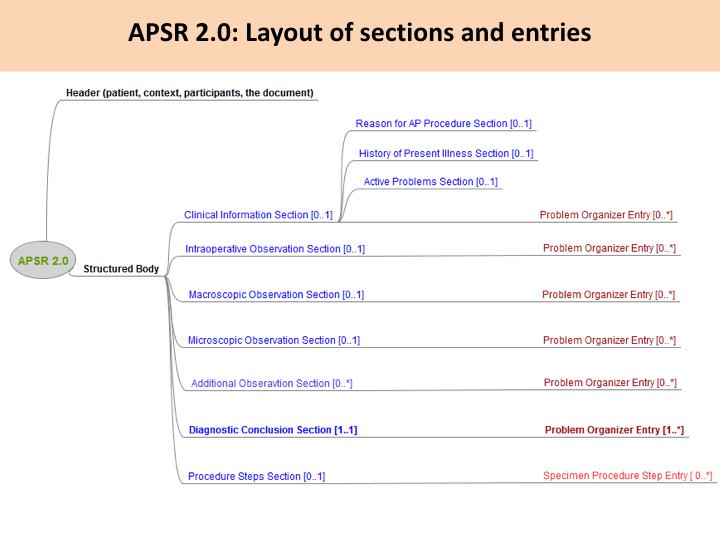
Figure 10.4.1-1
Common model for a digital anatomic pathology structured report
Note 1: The only section that is mandatory is
the Diagnostic Conclusion section.
10.4.2 Use Cases
10.4.2.1 Use case #1: Single Report
Anatomic pathology order fulfilled by a pathology laboratory produces a report.
10.4.2.1.1 Single Report Use Case Description
A surgeon removes a breast tumor from a patient, requests the procedure “breast surgical specimen - pathological examination” and sends the specimen(s) to the anatomic pathology laboratory.
Specimens) are accessioned by the anatomic pathology laboratory. The staff performs a macroscopic examination of the specimens ; gross imaging is performed if needed. The specimens are processed for microscopic examination and other special ancillary techniques or tissue banking if needed. During the imaging interpretation process, microscopic imaging is performed if needed. At the end of the interpretation process the pathologist queries the Content Creator application for the appropriate APSR template, fills the form, binds some relevant images and/or regions of interest to specific observations, validates and signs the digital report.
10.4.2.1.2 Single Report Process Flow
Intentionally left blank
10.4.2.1.3 Single Report Example
A. "RIGHT BREAST FIVE CORES 8-9:00" (ULTRASOUND GUIDED NEEDLE CORE BIOPSY):
INVASIVE ADENOCARCINOMA OF THE BREAST.
HISTOLOGIC TYPE: DUCTAL.
NOTTINGHAM COMBINED HISTOLOGIC GRADE: 1 OF 3.
TUBULE FORMATION SCORE: 2.
NUCLEAR PLEOMORPHISM SCORE: 2.
MITOTIC RATE SCORE: 1.
IN-SITU CARCINOMA: EQUIVOCAL.
BREAST CANCER BIOMARKER STUDIES:
PARAFFIN BLOCK NUMBER: A1.
ER INTERPRETATION: POSITIVE ESTROGEN RECEPTOR ACTIVITY (ALLRED SCORE = 8).
PR INTERPRETATION: POSITIVE PROGESTERONE RECEPTOR ACTIVITY (ALLRED SCORE = 8).
DAKO EGFR PHARMDX IMMUNOHISTOCHEMISTRY: NEGATIVE (0) FOR EXPRESSION OF
EPIDERMAL GROWTH FACTOR RECEPTOR.
HER2/NEU IMMUNOHISTOCHEMISTRY: POSITIVE (3+) FOR OVEREXPRESSION OF HER2/NEU
ONCOPROTEIN.
10.4.2.2 Use Case #2: Multi-step Report
Reporting includes multiple successive steps.
10.4.2.2.1 Multi-step Report Use Case Description
A surgeon removes a breast tumor from a patient, requests the procedure “breast surgical specimen - frozen sections & pathological examination”, and “breast surgical specimen - pathological examination” and sends the specimen(s) to the anatomic pathology laboratory.
Specimens are accessioned by the anatomic pathology department. The staff performs a macroscopic examination of the specimens, gross imaging is performed if needed. The specimens are processed for intraoperative observation if needed, and tissue banking if needed (e.g., for research purpose). During the imaging interpretation process of frozen sections, microscopic imaging is performed if needed. At the end of the interpretation process, the pathologist queries the Content Creator for the appropriate APSR template, fills the intraoperative observation section, binds some relevant images and/or regions of interest to specific observation(s) if needed, validates and signs (i.e., legally authenticates) the preliminary APSR.
The day after, the specimen(s) are processed for microscopic examination and other special ancillary techniques if needed. During the imaging interpretation process, microscopic imaging is performed if needed. At the end of the interpretation process, pathologist queries the Content Creator for the preliminary APSR, fills the form, binds some relevant images and/or regions of interest to specific observation(s), validates and signs (i.e., legally authenticates) the final APSR.
10.4.2.2.2 Multi-step Report Process Flow
Intentionally left blank
10.5 APSR Security Considerations
See Appendix A of PaLM TF-1.
10.6 APSR Cross Profile Considerations
Intentionally left blank
VOLUME 3 – CONTENT MODULES
1 Introduction
The content of this entire section is copied from section 1 of Volume 3 of PaLM TF.
1.1 Overview of the Anatomic Pathology Technical Framework
Integrating the Healthcare Enterprise (IHE) is an international initiative to promote the use of standards to achieve interoperability among health information technology (HIT) systems and effective use of electronic health records (EHRs). IHE provides a forum for care providers, HIT experts and other stakeholders in several clinical and operational domains to reach consensus on standards-based solutions to critical interoperability issues.
The primary output of IHE is system implementation guides, called IHE Profiles. IHE publishes each profile through a well-defined process of public review and trial implementation and gathers profiles that have reached final text status into an IHE Technical Framework, of which this volume is a part.
For more general information regarding IHE, refer to IHE International website. It is strongly recommended that, prior to reading this volume, the reader familiarizes themselves with the concepts defined in the IHE Technical Frameworks General Introduction.
1.2 Intended Audience
The intended audience of IHE Technical Frameworks Volume 3 is:
- IT departments of healthcare institutions
- Technical staff of vendors participating in the IHE initiative
- Experts involved in standards development
1.3 Overview of Technical Framework Volume 3
Volume 3 is comprised of several distinct sections:
- Section 1 provides background and reference material.
- Section 2 presents the conventions used in this volume to define the content modules.
- Section 3 provides an overview of Content Modules and the terminology used.
- Section 4 is reserved for domain unique Content Module specifications.
- Section 5 lists the namespaces and identifiers defined or referenced and the vocabularies defined or referenced herein.
- Section 6 defines the PaLM domain’s HL7 V3 CDA Content Modules in detail.
- Section 7 defines the PaLM domain’s DICOM content modules in detail.
- Section 8 defines other types of content modules.
The appendices in Volume 3 provide clarification of technical details of the IHE data model and transactions. A glossary of terms and acronyms used in the IHE Technical Framework, including those from relevant standards, is provided in the IHE Technical Frameworks General Introduction. Due to the length of the document, some domains may divide Volume 3 into smaller volumes labeled 3a, 3b, etc. In this case, the Volume 3 appendices are gathered in Volume 3x. Code and message samples may also be stored on the IHE ftp server. In this case, explicit links to the ftp server will be provided in the transaction text.
IHE International welcomes comments on this document and the IHE initiative. They can be submitted by sending an email to the co-chairs and secretary of the Pathology and Laboratory Medicine domain committees at palm@ihe.net
1.5 Copyright Licenses
IHE International hereby grants to each Member Organization, and to any other user of these documents, an irrevocable, worldwide, perpetual, royalty-free, nontransferable, nonexclusive, non-sublicensable license under its copyrights in any IHE profiles and Technical Framework documents, as well as any additional copyrighted materials that will be owned by IHE International and will be made available for use by Member Organizations, to reproduce and distribute (in any and all print, electronic or other means of reproduction, storage or transmission) such IHE Technical Documents.
The licenses covered by this Copyright License are only to those copyrights owned or controlled by IHE International itself. If parts of the Technical Framework are included in products that also include materials owned or controlled by other parties, licenses to use those products are beyond the scope of this IHE document and would have to be obtained from that other party.
1.5.1 Copyright of Base Standards
IHE technical documents refer to and make use of a number of standards developed and published by several standards development organizations. All rights for their respective base standards are reserved by these organizations. This agreement does not supersede any copyright provisions applicable to such base standards.
Health Level Seven, Inc. has granted permission to IHE to reproduce tables from the HL7 standard. The HL7 tables in this document are copyrighted by Health Level Seven, Inc. All rights reserved. Material drawn from these documents is credited where used.
1.6 Trademark
IHE® and the IHE logo are trademarks of the Healthcare Information Management Systems Society in the United States and trademarks of IHE Europe in the European Community. They may only be used with the written consent of the IHE International Board Operations Committee, which may be given to a Member Organization in broad terms for any use that is consistent with the IHE mission and operating principles.
1.7 Disclaimer Regarding Patent Rights
Attention is called to the possibility that implementation of the specifications in this document may require use of subject matter covered by patent rights. By publication of this document, no position is taken with respect to the existence or validity of any patent rights in connection therewith. IHE International is not responsible for identifying Necessary Patent Claims for which a license may be required, for conducting inquiries into the legal validity or scope of Patents Claims or determining whether any licensing terms or conditions provided in connection with submission of a Letter of Assurance, if any, or in any licensing agreements are reasonable or non-discriminatory. Users of the specifications in this document are expressly advised that determination of the validity of any patent rights, and the risk of infringement of such rights, is entirely their own responsibility. Further information about the IHE International patent disclosure process including links to forms for making disclosures is available here. Please address questions about the patent disclosure process to the secretary of the IHE International Board: secretary@ihe.net
1.8 History of Document Changes
Content Modules for the APSR 2.0 Profile:
- Reconfiguration of the Document content module
- Reconfiguration of the Procedure step section content module
- Introduction of the Additionally Specified Observation section content module
- Reconfiguration of the entry content modules "Problem organizer" and "Specimen procedure steps"
- Introduction of child element content modules "X-specimen identified", "UICC/AJCC-TNM observation", "ICD-O-3 observation", "Assessment scales observation"
- Renewal and completion of value sets.
Transformation of a real-world use case into a valid APSR 2.0 xml instance.
Finishing the Supplement ready to public comment.
2 Conventions
This document has adopted the following conventions for representing the framework concepts and specifying how the standards upon which the IHE Technical Framework is based shall be applied.
2.1 Content Module Modeling and Profiling Conventions
In order to maintain consistent documentation, modeling methods for IHE content modules and profiling conventions for frequently used standards are maintained as an appendix in the IHE Technical Frameworks General Introduction. Methods described include the standards conventions DICOM, HL7 v2.x, HL7 Clinical Document Architecture (CDA) Documents, etc. These conventions are critical to understanding this volume and should be reviewed prior to reading this text.
2.2 Additional Standards Profiling Conventions
This section defines profiling conventions for standards which are not described in the IHE Technical Frameworks General Introduction.
Not Applicable.
3 Content Modules Overview and Terminology
In the future, an appendix to the IHE Technical Frameworks General Introduction will provide an overview of Content Modules. In the interim, information may be available here.
The Pathology and Laboratory Medicine content modules are listed in the table below:
Table 3-1: Pathology and Laboratory Medicine Content Modules
| Content Module Acronym |
Type of Content Modules |
Semantic |
Status
|
| XD-LAB |
CDA R2 medical document |
Clinical Laboratory Structured Report |
Final Text
|
| APSR |
CDA R2 medical document |
Anatomic Pathology Structured Report |
Public Comment
|
4 to be cleaned
This Volume 3 of
the Suppl. APSR 2.0 to the PaLM TF organizes content modules categorically by the base standard. At
present, former PAT TF-3 uses only one base standard, CDA Release 2.0, but this is
expected to change over time. Underneath each standard, the content modules are
organized using a very coarse hierarchy inherent to the standard.
Each content
module can be viewed as the definition of a "class" in software
design terms, and has associated with it a name. Like "class"
definitions in software design, a content module is a "contract", and
the former PAT TF-3 defines that contract in terms of constraints that must be obeyed
by instances of that content module. Each content module has a name, also known
as its template identifier. The template identifiers are used to identify the
contract agreed to by the content module. The Pathology and Laboratory Medicine Technical Committee is responsible for assigning the template identifiers to each content module.
Like classes,
content modules may inherit features of other content modules of the same type
(e.g., Document, Section or Entry) by defining the parent content module that
they inherit from. They may not inherit features from a different type.
Constraints that
apply to any content module will always apply to any content modules that
inherit from it. Thus, the "contracts" are always valid down the
inheritance hierarchy.
The former PAT TF-3 uses
the convention that a content module cannot have more than one parent (although
it may have several ancestors). This convention is not due to any specific
technical limitation of the technical framework, but does make it easier for
software developers to implement content modules.
Each content
module has a list of data elements that are required (R), required if known
(R2), conditional (C) or optional (O).
Other data
elements may be included in an instance of a content module over what is
defined by the former PAT TF-3. Content consumers are not required to process these elements, and if they do not understand them, must ignore them. Thus, it is not an error to include more than is asked for, but it is an error to reject a
content module because it contains more than is defined by the framework. This
allows value to be added to the content modules delivered internationally in
this framework, through national extensions built by the national IHE
organizations in various countries. It further allows content modules to be
defined later by IHE that are refinements or improvements over previous content
modules.
3 IHE Transactions
This section
defines each IHE transaction in detail, specifying the standards used, and the
information transferred.
3.1 Cross Enterprise Document Content Transactions
At present, all
transactions used by the Anatomic Pathology Content Profiles appear in ITI TF-2a
and ITI TF-2b.
General Options
defined in content profiles for a Content Consumer are listed below.
3.1.1 View Option
A Content
Consumer that supports the View Option shall be able to:
1. Use the appropriate XD* transactions to obtain the document along with associated
necessary metadata.
2. Render the document for viewing. This rendering shall meet the requirements defined
for CDA Release 2 content presentation semantics (See Section 1.2.4 of the CDA
Specification: Human readability and rendering CDA Documents). CDA Header
information providing context critical information shall also be rendered in a
human readable manner. This includes at a minimum the ability to render the
document with the stylesheet specifications provided by the document source, if
the document source provides a stylesheet. Content Consumers may optionally
view the document with their own stylesheet, but must provide a mechanism to
view using the source stylesheet.
3. Support traversal of links for documents that contain links to other documents managed
within the sharing framework.
4. Print the document to paper.
3.1.2 Document Import Option
This Option
requires that the View Option be supported. In addition, the Content Consumer
that supports the Document Import Option shall be able to support the storage
of the entire APSR document (as provided by the sharing framework, along with
sufficient metadata to ensure its later viewing). The machine-readable content
(from the entry elements) shall also be imported. This Option requires the
proper tracking of the document origin. Once a document has been imported, the
Content Consumer shall offer a means to view the document without the need to
retrieve it again from the sharing framework. When the document is used after
it was imported, a Content Consumer may choose to access the sharing framework
to find out if the related Document viewed has been deprecated or replaced.
3.1.3 Section Import Option
This Option
requires that the View Option be supported. In addition, the Content Consumer
that supports the Section Import Option shall be able to support the import of
one or more sections of the APSR document (along with sufficient metadata to
link the data to its source). The machine-readable content (from the entry
elements beneath the imported sections) shall also be imported. This Option
requires the proper tracking of the document section origin. Once sections have
been selected, a Content Consumer shall offer a means to copy the imported
section(s) into local data structures. When a section is used after it is
imported, a Content Consumer may choose to access the sharing framework to find
out if the related information has been updated.
4 IHE Anatomic Pathology Bindings
This section
describes how the payload used in a transaction of an IHE profile is related to
and/or constrains the data elements sent or received in those transactions.
This section is where any specific dependencies between the content and
transaction are defined.
A content profile
can define multiple bindings. Each binding should identify the transactions and
content to which it applies.
The source for
all required and optional attributes have been defined in the bindings below.
Three tables describe the three main XDS object types: XDSDocumentEntry,
XDSSubmissionSet, and XDSFolder. XDSSubmissionSet and XDSDocumentEntry are
required. Use of XDSFolder is optional. These concepts are universal to XDS,
XDR and XDM.
The structure of
these three tables is presented in PCC TF-2:4
4.1 Anatomic Pathology Document Binding to XDS, XDM and XDR
This binding
defines a transformation that generates metadata for the XDSDocumentEntry element of appropriate transactions from the XDS,
XDM and XDR profiles given a medical document and information from other
sources. The medical document refers to the document being stored in a
repository that will be referenced in the registry. The other sources of
information include the configuration of the Document Source actor, the
Affinity Domain, the site or facility, local agreements, other documents in the
registry/repository, and this content profile.
In many cases,
the CDA document is created for the purposes of sharing within an affinity
domain. In these cases the context of the CDA and the context of the affinity
domain are the same, in which case the following mappings shall apply.
In other cases,
the CDA document may have been created for internal use, and are subsequently
being shared. In these cases the context of the CDA document would not necessarily
coincide with that of the affinity domain, and the mappings below would not
necessarily apply.
4.1.1XDS DocumentEntry Metadata
The general table
describing the XDSDocumentEntry Metadata requirements for IHE domains is shown in PCC TF-2:4.1.1
The sub-sections
below list the only requirements which are specific to the Anatomic Pathology
Domain, and which supersede those from the general table mentioned above.
4.1.1.1XDS DocumentEntry.formatCode
The values of formatCode per document template are
listed in chapter 5.6.
The associated codingScheme Slot SHALL be 1.3.6.1.4.1.19376.1.2.3 in all cases.
4.1.1.2XDS DocumentEntry.eventCodeList
This metadata
provides a means to index anatomic pathology reports by reportable conditions (e.g.,
certain types of tumors…) so as to facilitate later queries in a registry of
shared clinical documents. The conclusions coded in the entry element of the Diagnostic Conclusion section are good
candidates for this metadata.
4.1.1.3XDS DocumentEntry.parentDocumentRelationship
The Anatomic
Pathology document Content Modules only permit the “replace” relationship
between instances of APSR documents.
Thus, XDSDocumentEntry.parentDocumentRelationship
is constrained to the "RPLC" (replace) value. The new document issued replaces completely the parent one, which will be considered as deprecated.
4.1.2XDS SubmissionSet Metadata
The submission
set metadata is as defined for XDS, and is not necessarily affected by the
content of the clinical document. Metadata values in an XDSSubmissionSet with names identical to those in the XDSDocumentEntry may be inherited from XDSDocumentEntry metadata, but this is
left to affinity domain policy and/or application configuration.
This content
format uses the submission set to create a package of information to send from
one provider to another. All documents or images referenced by the Anatomic
Pathology Structured Report in this Package must be present (at least as
references in the case of images) in the submission set.
4.1.3XDS Folder Metadata
No specific requirements identified.
4.1.4 Configuration
The Anatomic
Pathology Content Profiles using this binding require that Content Creators and
Content Consumers be configurable with institution and other specific
attributes or parameters. Implementers should be aware of these requirements to
make such attributes easily configurable.
5 Namespaces and Vocabularies
5.1 OID tree of PAT TF
1.3.6.1.4.1.19376.1.81.3.6.1.4.1.19376.1.8 is the OID of the former IHE Anatomic Pathology domain, whereas 1.3.6.1.4.1.19376.1.81.3.6.1.4.1.19376.1.3 is the OID for PaLM domain :
All exchangeable objects specified by these domains are identified by OIDs built on these roots:
Branch 1.3.6.1.4.1.19376.1.8.1 is dedicated to CDA Content Modules created by the AP domain
Sub-branch 1.3.6.1.4.1.19376.1.8.1.1 is the OID of the generic Document Content Module
Sub-branch 1.3.6.1.4.1.19376.1.8.1.2 is dedicated to Section Content Modules
Sub-branch 1.3.6.1.4.1.19376.1.8.1.3 is dedicated to Entry Content Modules.
Sub-branch 1.3.6.1.4.1.19376.1.8.1.3.6 is the OID of the Problem Organizer
Sub-branch 1.3.6.1.4.1.19376.1.8.1.4 is dedicated to Element Content Modules
Sub-branch 1.3.6.1.4.1.19376.1.8.1.4.9 is the OID of the generic anatomic pathology (AP) observation template
Branch 1.3.6.1.4.1.19376.1.8.2 is dedicated to terminologies defined by AP domain
Sub-branch 1.3.6.1.4.1.19376.1.8.2.1 is dedicated to PathLex
Branch 1.3.6.1.4.1.19376.1.8.5 is dedicated to Value Sets defined by AP domain.
Branch 1.3.6.1.4.1.19376.1.3.10 is dedicated to Templates newly defined by PaLM domain.
Sub-branch 1.3.6.1.4.1.19376.1.3.10.1 is dedicated to CDA Document Level Templates
Sub-branch 1.3.6.1.4.1.19376.1.3.10.2 is dedicated to CDA Header Level Templates
Sub-branch 1.3.6.1.4.1.19376.1.3.10.3 is dedicated to CDA Section Level Templates
Sub-branch 1.3.6.1.4.1.19376.1.3.10.4 is dedicated to CDA Entry Level Templates
Sub-branch 1.3.6.1.4.1.19376.1.3.10.9 is dedicated to CDA Template Fragments/Supporting Templates
Branch 1.3.6.1.4.1.19376.1.3.11 is dedicated to Value Sets newly defined by PaLM domain.
Branch 1.3.6.1.4.1.19376.1.8.9 is used to identify instances in the examples built by the AP domain.
Notes on other IHE OIDs used in the AP domain:
nn
5.2 Terminologies and controlled coded vocabularies
This section lists the terminologies and the coded vocabularies referenced by this Volume 3.
Table 5.2-1 Anatomic Pathology Terminologies and Coded Vocabularies
 |
Could this be contributed by ArtDecor??? GH |
| codeSystem |
codeSystemName |
Description |
Owner
|
| 2.16.840.1.113883.6.1
|
LOINC
|
Logical Observation Identifier Names and Codes
|
Regenstrief Institute
|
| 2.16.840.1.113883.6.8
|
UCUM
|
Unified Code for Units of Measure
|
Regenstrief Institute, and the UCUM Organization
|
| 2.16.840.1.113883.6.96
|
SNOMED-CT |
Systematized Nomenclature of Medicine – Clinical Terms
|
IHTSDO
|
| 1.3.6.1.4.1.19376.1.5.3.2
|
IHEActCode |
Vocabulary defined by IHE PCC in PCC TF-2:5.1.2, used for representing annotation comments in the report
|
IHE PCC
|
| 2.16.840.1.113883.5.4
|
Act Code |
Codesystem for Acts
|
HL7
|
| 2.16.840.1.113883.5.6
|
ActClass |
Codesystem for Act Classes
|
HL7
|
| 2.16.840.1.113883.5.1052
|
Act Site |
Codesystem for Act Sites
|
HL7
|
| 2.16.840.1.113883.5.1065
|
ProcedureMethod |
Codesystem for Procedure Methods
|
HL7
|
| 2.16.840.1.113883.5.111
|
Role Code |
Codesystem for Role Codes
|
HL7
|
| 2.16.840.1.113883.5.129
|
SpecimenType |
Codesystem for Specimen Types
|
HL7
|
| 2.16.840.1.113883.5.84
|
ObservationMethod |
A code system that provides additional detail about the means or technique used to ascertain the observation
|
HL7
|
| 2.16.840.1.113883.6.3
|
ICD-10 |
International Classification of Diseases revision 10
|
WHO
|
| 2.16.840.1.113883.6.43
|
ICD-O-3 |
International Classification of Diseases for Oncology revision 3
|
WHO
|
| 1.2.840.10008.2.16.4
|
DICOM controlled vocabulary |
The meanings of codes defined in DICOM, either explicitly or by reference to another part of DICOM or an external reference document or standard [2]
|
DICOM
|
| 1.2.250.1.213.2.11
|
ADICAP Thesaurus |
French thesaurus of lesions in anatomic pathology - not used in APSR 2.0. Replaced by SNOMED CT
|
ADICAP
|
| 1.2.250.1.213.2.12
|
SNOMED International (3.5) |
Systematized Nomenclature of Medicine - no longer usable. Replaced by SNOMED CT, the only valid version.
|
ASIP santé
|
| 1.3.6.1.4.1.19376.1.8.2.1
|
PathLex |
Temporary terminology covering the scope of anatomic pathology observation results and specimen collection procedure code. No longer used. Replaced by SNOMED CT.
|
IHE-PAT
|
| 2.16.840.1.113883.15.6
|
TNM 7th edition |
Internationally agreed-upon standards to describe and categorize cancer stages and progression http://www.uicc.org/resources/tnm
|
Union for International Cancer Control (UICC) & American Joint Committee on Cancer (AJCC)
|
| 2.16.840.1.113883.15.7
|
TNM 6th edition |
Internationally agreed-upon standards to describe and categorize cancer stages and progression http://www.uicc.org/resources/tnm
|
Union for International Cancer Control (UICC) & American Joint Committee on Cancer (AJCC)
|
| 2.16.840.1.113883.15.8
|
TNM 5th edition |
Internationally agreed-upon standards to describe and categorize cancer stages and progression http://www.uicc.org/resources/tnm
|
Union for International Cancer Control (UICC) & American Joint Committee on Cancer (AJCC)
|
| 2.16.840.1.113883.6.4
|
ICD-10-PCS |
International Classification of Diseases, 10th Revision, Procedure Coding System (ICD-10-PCS)
|
WHO
|
| 1.2.276.0.76.5.464
|
OPS 2017 |
Code lists to describe and categorize surgeries and procedures, adapted from WHO ICPM for Germany
|
DIMDI (WHO)
|
| 2.16.840.1.113883.6.174
|
OMIM |
Code lists to describe and categorize human genes. OMIM is a comprehensive, authoritative compendium of human genes and genetic phenotypes that is freely available and updated daily.
|
OMIM Johns Hopkins University School of Medicine [3]
|
| 1.2.276.0.76.3.1.131.1.5.1
|
DKG Coding Scheme |
Internationally agreed-upon code lists to describe and categorize cancer grading systems, adapted for Germany [4]
|
DKG (Deutsche Krebsgesellschaft)
|
| 1.2.276.0.76.5.336
|
Grading / Differentiation scheme |
Code lists to describe and categorize Tumor grading according ICD-O-3, adapted for Germany
|
HL7.de
|
| 1.2.276.0.76.5.401
|
Localization scheme for distant metastases |
Code lists to describe and categorize localization of metastases according UICC, adapted for Germany
|
HL7.de
|
5.3 Value Sets
The value sets defined or referenced by this Volume 3 of the IHE PaLM TF Suppl. are listed in Volume 4.
5.4 Namespaces
5.4.1 Namespace protecting extensions to the CDA schema
There is currently one single extension to the CDA.xsd schema used in PAT TF-3. This extension has been created by IHE LAB and is protected by this particular namespace in document instances: xmlns:lab="urn:oid:1.3.6.1.4.1.19376.1.3.2"
5.5 References to Content Modules built outside of IHE PAT TF
The Content Modules specified in this Volume 3 of the PAT TF leverage a number of Content Modules (currently CDA templates) produced and maintained by other groups, including other domains of IHE. Table 5.5-1 lists them.
Table 5.5-1 External Content Modules referenced by PAT TF-3
| templateId |
Standard |
Definition |
Source of Specification
|
| 1.3.6.1.4.1.19376.1.5.3.1.3.1 |
CDA R2
|
Reason for referral
|
IHE PCC TF-2:6.3.3.1.2
|
| 1.3.6.1.4.1.19376.1.5.3.1.3.4
|
CDA R2 |
History of present illness
|
IHE PCC TF-2:6.3.3.2.1
|
| 1.3.6.1.4.1.19376.1.5.3.1.3.6
|
CDA R2 |
Active Problems
|
IHE PCC TF-2:6.3.3.2.3
|
| 1.3.6.1.4.1.19376.1.5.3.1.4.2
|
CDA R2 |
Annotation Comment
|
IHE PCC TF-2:6.3.4.6
|
| 1.3.6.1.4.1.19376.1.3.3.1.7
|
CDA R2 |
Laboratory Performer
|
IHE PaLM TF-3:6.3.2.20
|
| 1.3.6.1.4.1.19376.1.3.3.1.6
|
CDA R2 |
Ordering Provider (ordering physician)
|
IHE PaLM TF-3:6.3.2.17
|
| 1.3.6.1.4.1.19376.1.3.3.1.4
|
CDA R2 |
Intended Recipient
|
IHE PaLM TF-3:6.3.2.14
|
| 1.3.6.1.4.1.19376.1.3.1.6
|
CDA R2 |
Laboratory Observation
|
IHE PaLM TF-3:6.3.4.13
|
5.6 IHE Codes for Anatomic Pathology Document Templates
Any AP structured report SHALL conform to the APSR generic Content Module Identified by templateId “1.3.6.1.4.1.19376.1.8.1.1.1” , and SHALL be associated with the following metadata:
- typeCode = “11526-1”, which is the LOINC code for “Pathology study”.
- formatCode = “urn:ihe:pat:apsr:all:2010”, with associated codingScheme = “1.3.6.1.4.1.19376.1.2.3” as assigned by the ITI Domain for codes used for the purposes of cross-enterprise document sharing (XDS).
- The media type SHALL be “text/xml”.
6 Anatomic Pathology Content Modules
6.1 Conventions
In all Content Modules specified in this section, the abbreviation “AP” stands for “Anatomic Pathology”.
Various tables used in this section will further constrain the content. Within this volume, the following conventions are used:
M (R in v2)
A "Mandatory (Required in v2)" data element is one that shall always be provided. If there is information available, the data element must be present. If there is no information available, or it cannot be transmitted, the data element must contain a value indicating the reason for omission of the data.
R (R2 in v2)
A "Required (Required if data present in v2)" data element is one that shall be provided when a value exists. If the information cannot be transmitted, the data element shall contain a value indicating the reason for omission of the data. If no such information is available to the content creator or if such information is not available in a well identified manner (e.g., buried in a free form narrative that contains additional information relevant to other sections) or if the content creator requires that information be absent, the R2 section shall be entirely absent. The Content Creator application must be able to demonstrate that it can populate all required if known elements, unless it does not in fact gather that data. This “R2” code is the equivalent of the HL7 standard “RE” usage code. The value “R2” has been chosen in harmonization with the IHE PCC TF, which is the source of a large number of CDA R2 content modules.
O
An "Optional" data element is one that may be provided, irrespective of whether the information is available or not. If the implementation elects to support this optional section, then its support shall meet the requirement set forth for the "Required if data present" or R2.
C
A "Conditional" data element is one that is required, required if known or optional depending upon other conditions. These will have further notes explaining when the data element is required, et cetera.
6.2 HL7 CDA R2 Content Modules
6.2.1 Organization
6.2.1.1 Various Types of Content Modules
For the CDA Release 2.0 standard, the content modules are organized by:
- document: The template for a whole document.
- section: The template for a <section> element.
- entry: The template for a <entry> element.
- child element: An element of the CDA header or an element of a <section>, or an element nested at various depths below an <entry>, or an element appearing at some combination of these locations.
6.2.1.2 General constraints added by IHE PAT to a CDA R2 document
In the structured body of a CDA R2 document, a section has a narrative block (the text element), which presents the human-readable content of the section, and MAY have one entry or more. Sections MAY be nested within one another.
The content modules designed by the PAT TF bring or highlight the following constraints:
- When a section has a text element and one or more entry element, the content coded for machine-processing in the entries SHALL be completely transcribed into human-readable content in the text element.
- Conversely the text element MAY contain pieces of information, which are not available in machine-readable format in any entry element of the section.
- For a document of the Anatomic Pathology domain, the entry elements are instantiated per specimen or per group of specimens observed together. One entry contains in machine-readable format observations of the section related to the same specimen or group of specimens. Beneath an entry, the observations are organized per problem.
- The text element of the section is supposed to be also laid out per specimen or group of specimens and per problem observed.
- The APSR Content Profile leaves the layout of the text element up to the Content Creator applications, or to further constraints brought by national extensions of this profile. However, given that the text element is usually composed of free text (e.g. dictated text), assembled with the text generated from the set of data, machine-encoded in the entry elements below, the Content Creator application MUST handle these two kinds of content, and provide a user interface, which avoids risks of overwriting text automatically derived from the entries with free text typed in by the user (e.g., using forms with dedicated free text areas and distinct protected areas for text generated out of structured data).
- Information that is sent SHALL clearly identify distinctions between:
None
It is known with complete confidence that there are none. This indicates that the sender knows that there is no relevant information of this kind that can be sent.
None Known
None known at this time, but it is not known with complete confidence that none exist.
Asked but unknown
The information was requested but could not be obtained. Used mainly in the context where an observation was made but the result could not be determined.
Unknown
The information is not known, or is otherwise unavailable.
Other, not specified
The actual value does not belong to the assigned value set and is not reported at all by the author.
Other, specify
The actual value does not belong to the assigned value set and the author of the report provides this foreign value anyway.
Not applicable
No proper value is applicable in this context.
Sections that are required to be present but have no information should use one of the above phrases where appropriate in the text element.
Structural elements that are required but have no information shall provide a “nullFlavor” attribute coding the reason why the information is missing.
| Situation |
nullFlavor |
HL7 Definition
|
| Asked but unknown |
ASKU
|
Information was sought but not found
|
| Unknown
|
UNK |
A proper value is applicable, but not known
|
| Other, not specified
|
OTH |
The actual value is not an element in the value domain of a variable. (e.g., concept not provided by required code system).
|
| Not applicable
|
NA |
No proper value is applicable in this context
|
| Temporarily not available
|
NAV |
Information is not available at this time but it is expected that it will be available later.
|
The two situations “None” and “None known” represent effective values, which are part of the related value sets.
The situation “Other, specify” can be handled in two ways in a coded data element:
- Leaving empty the code attribute and providing the non-coded answer in the originalText attribute.
- Providing a value coded from a different coding scheme, when the coding strength of the element is “CWE” (coded with extensions). The attributes code, displayName, codeSystem and codeSystemName then describe the foreign code.
For ancillary techniques, the situation “ not performed” or “none performed” is represented by nullFlavor = NAV.
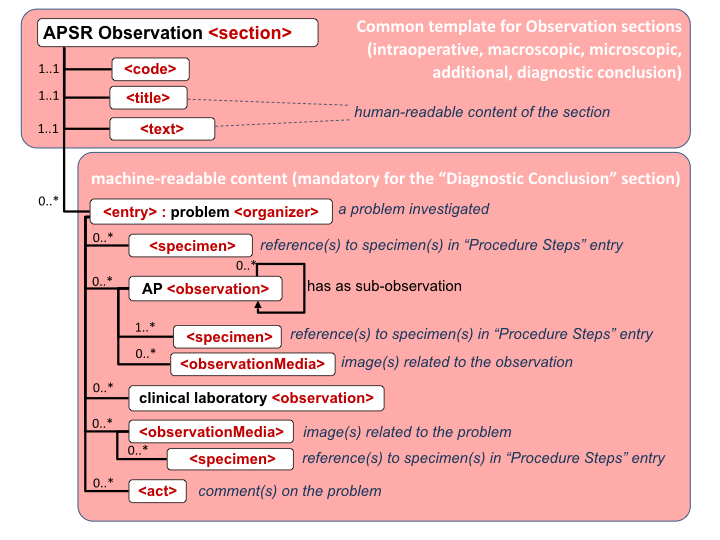
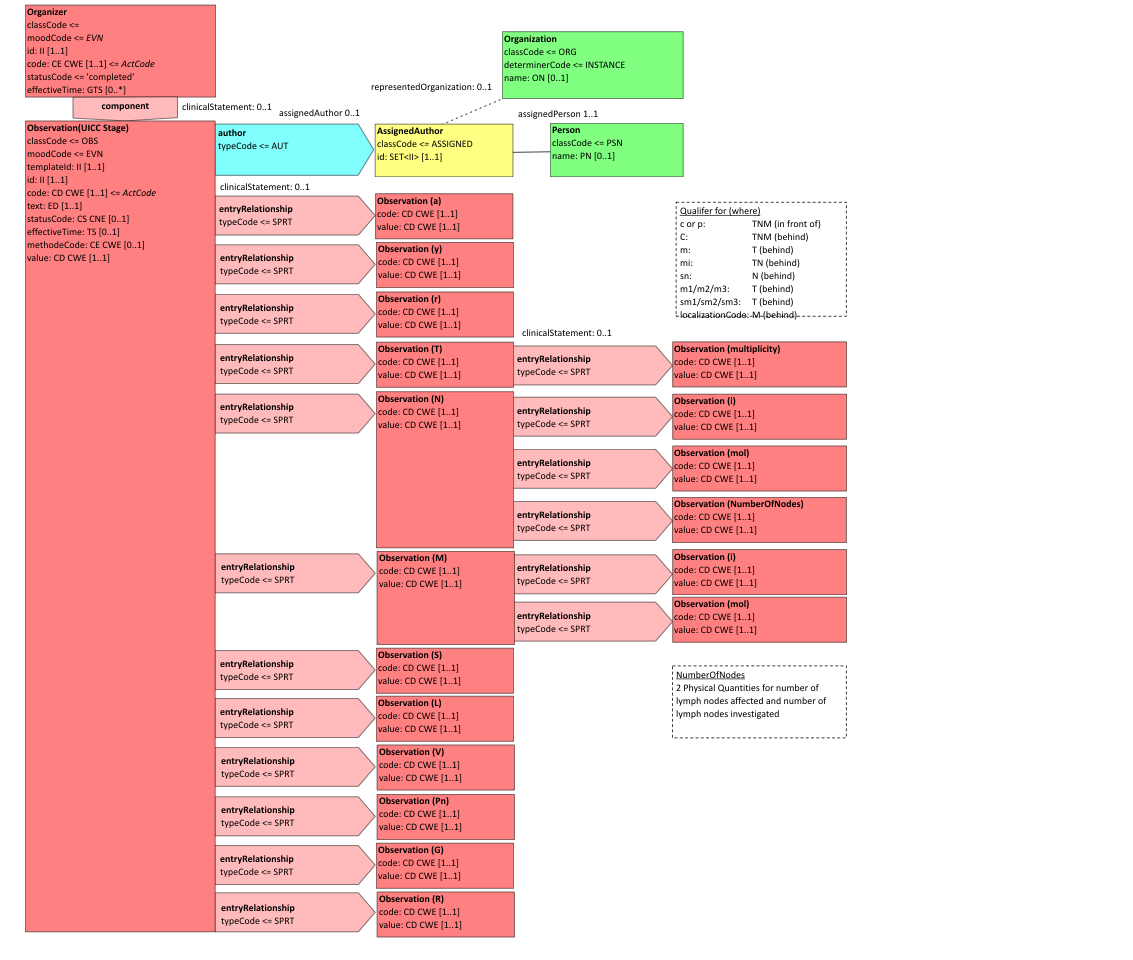
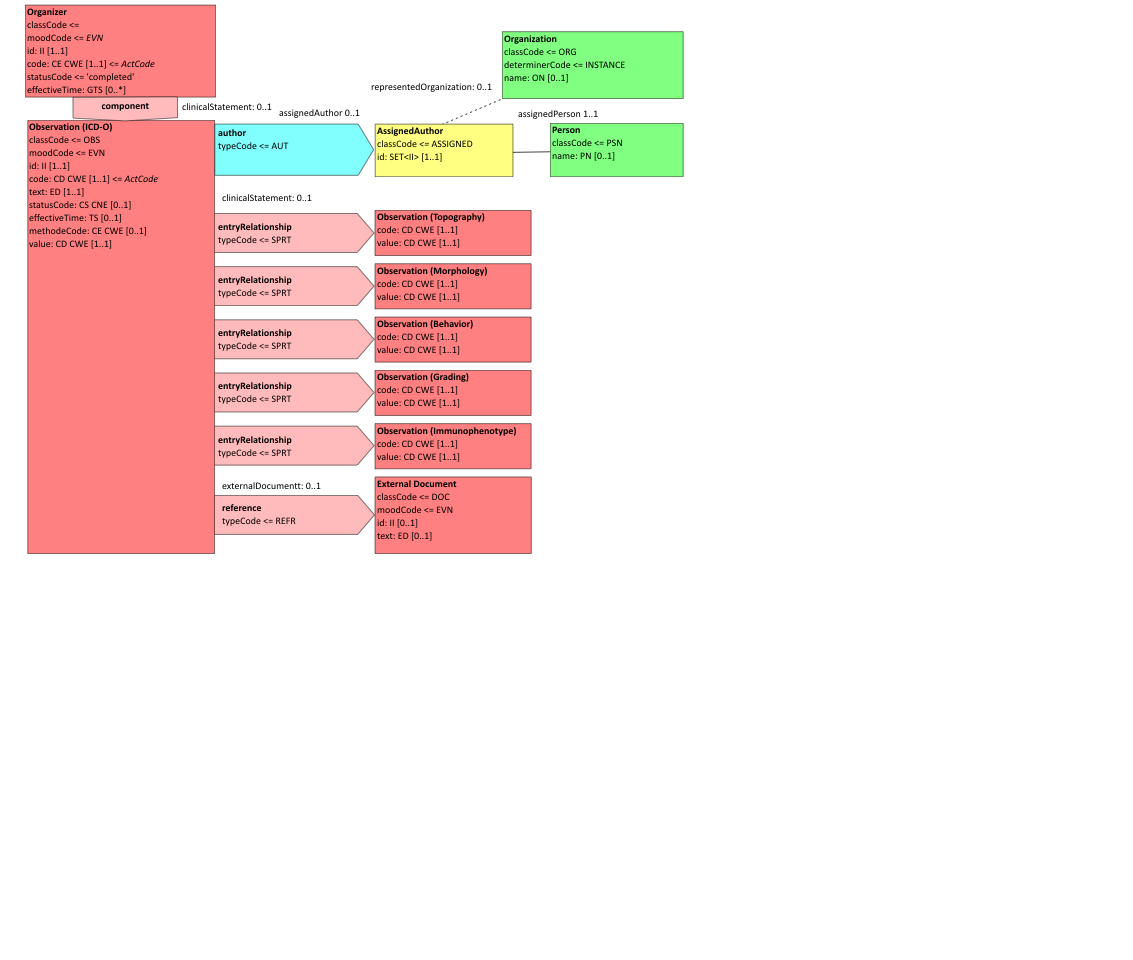
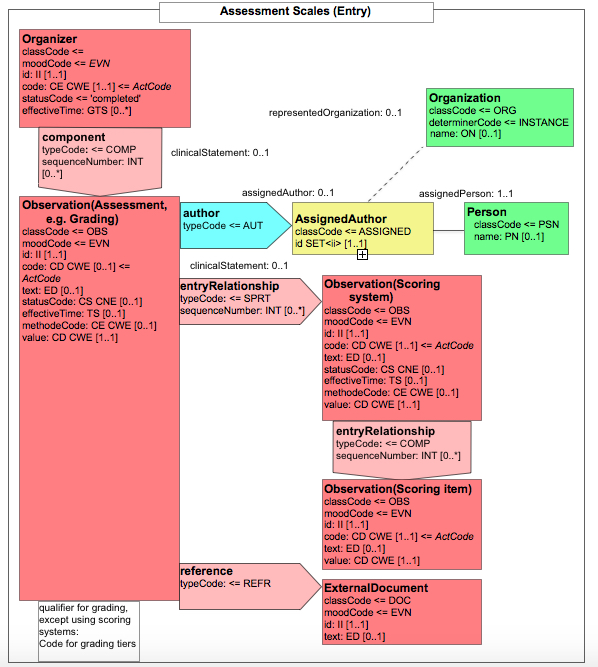
6.2.1.3 Common structure for CDA APSR
Figure 6.2.1.3-1 summarizes the common structure of the first six CDA APSR Section Content Modules specified here. Regarding the machine-readable part, the figure highlights the organization of entries within a section and of observations within an entry. Specific details such as the structure of sub-sections are not shown on this global picture.
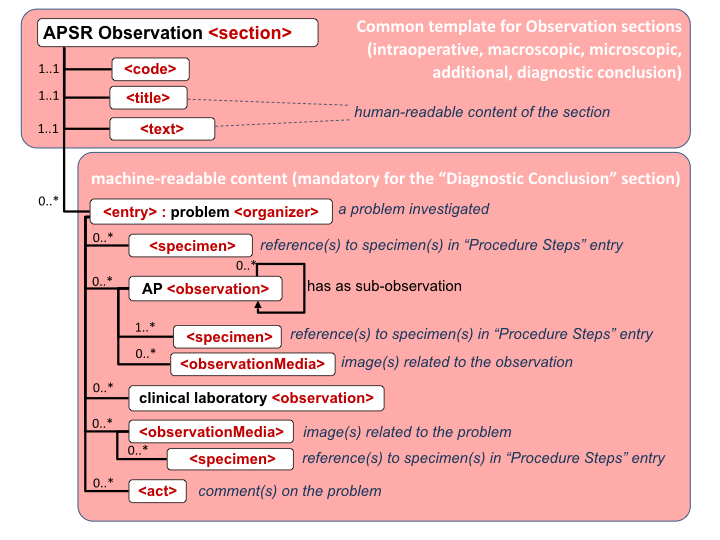
Figure 6.2.1.3-1 CDA APSR: common structure of machine-readable content for CDA APSR Section Content Modules except Procedure Step Content Module
Note 1: In order to facilitate a further de-identification process of CDA AP reports for some secondary use (biosurveillance, epidemiology…) the producer of an APSR SHOULD avoid populating any patient identification data (name, sex, birthdate, address …) into the body of the report (neither <entry> elements nor <text> elements). The appropriate location for patient identification data is the CDA header exclusively.
Note 2: The AP sections are those shown on figure 10.4.1-1 of Volume 1.
Note 3: The possible sub sections are shown on figure 10.4.1-1 of Volume 1.
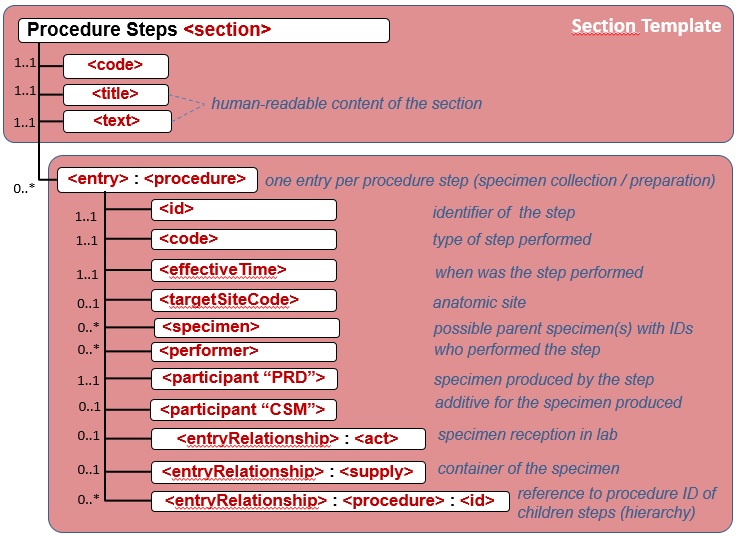
Figure 6.2.1.3-2 shows the common structure of the Procedure Step Content Module specified here, too.
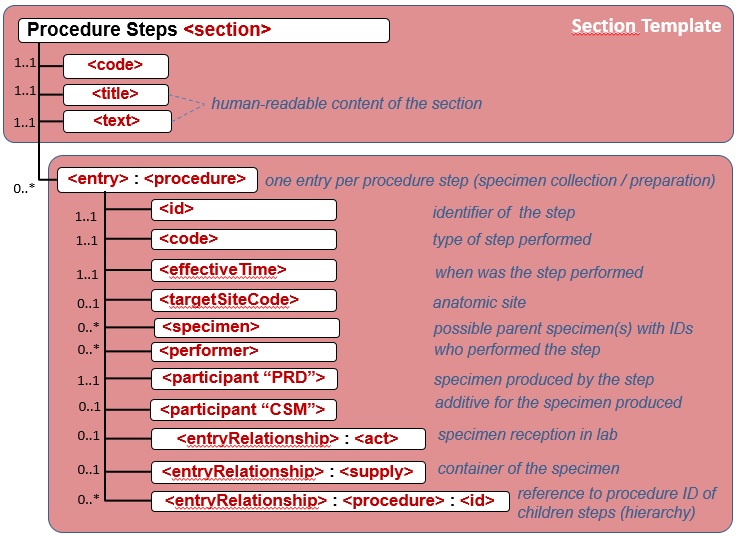
Figure 6.2.1.3-2 CDA APSR: common structure of machine-readable content for Procedure Step Content Module
6.2.2 Common layout for the specification of a CDA Content Module
Each CDA R2 Content Module specified in this Volume is presented with this layout:
6.2.2.1 Content Module Name – OID
Each Content Module is uniquely identified by a unique OID.
6.2.2.1.1 Definition and purpose
This section presents the content module and its purpose.
In case this module is a specialization of a more generic one, the section references its parent template.
6.2.2.1.2 Specification and example
This section consists of a transclusion of an Art-Decor APSR 2.0 template for the content module, delivering a snippet, showing an example of the content module.
The form of the specification depends upon the kind of CDA Content Module (document, section, entry, header and/or entry element). It respects the guidelines below:
- The specification provides a table describing the structure of the content module, each element being located through an XPATH expression combined with indentation. The table provides cardinalities, meaning for each elements, references value sets described in section 5 for attributes, and provides the mapping with HL7 V2.5.1 relevant fields. The table also points the content modules nested in the current one, by showing their templateId, and locating their specification in the current PAT TF-3 or in the IHE TF they belong to (PCC, LAB, etc.).
- The table is simplified for section content modules: It only lists the content modules nested in the section template.
- Within the tables appear notes providing additional information and detailing particular constraints on some elements or attributes.
6.2.3 CDA R2 Document Content Modules
6.2.3.1 AP Structured Report (APSR) - 1.3.6.1.4.1.19376.1.8.1.1.1
6.2.3.1.1 Definition and purpose
This Document Content Module defines the base set of constraints that apply to all AP structured report, related to any kind of lesion or diagnostic. In other words, this is the generic template for any AP structured report.
The body of this Document Content Module has the hierarchy of sections and entries depicted by figure 4.1.2.1-1 in Volume 1.
6.2.3.1.2 Specification and Example
| Id | 1.3.6.1.4.1.19376.1.8.1.1.1 | Effective Date | valid from 2014‑05‑13 11:57:57 |
|---|
| Status |  Draft Draft | Version Label | 2.0 |
|---|
| Name | AnatomicPathologyStructuredReportContentModule | Display Name | Anatomic Pathology Structured Report Content Module |
|---|
| Description | Anatomic Pathology Structured Report Content Module.
This document content module represents the generic set of constraints applied to any structured report for surgical pathology in all fields of anatomic pathology (cancers, benign neoplasms as well as non-neoplastic conditions) as well as for Cytopathology.
The body of this Document Content Module specifies a common hierarchy of sections and entries depicted by figure 10.4.1-1 in Volume 1 IHE_PaLM_Suppl_APSR 2.0. The only mandatory section is the Diagnostic Conclusion Section. And the only mandatory entry is the Problem Organizer Entry below this section.
|
|
| Context | Pathname / |
|---|
| Label | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module
|
|---|
| Classification | CDA Document Level Template |
|---|
| Open/Closed | Open (other than defined elements are allowed) |
|---|
| Used by / Uses | | Used by 0 transactions and 0 templates, Uses 20 templates | | Uses | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.3.3.1.1 | Include |  Human Patient (2017) Human Patient (2017) | 2017‑06‑07 | | 1.3.6.1.4.1.19376.1.8.1.4.2 | Include |  CDA author IHE CDA author IHE | 2016‑06‑21 14:02:11 | | 2.16.840.1.113883.10.12.103 | Include |  CDA dataEnterer CDA dataEnterer | 2005‑09‑07 | | 1.3.6.1.4.1.19376.1.8.1.4.6 | Containment |  CDA Informant(Header&Body) APSR2 (2.0) CDA Informant(Header&Body) APSR2 (2.0) | 2016‑07‑08 11:22:58 | | 2.16.840.1.113883.10.12.104 | Include |  CDA custodian CDA custodian | 2005‑09‑07 | | 1.3.6.1.4.1.19376.1.3.3.1.4 | Include |  XD-LAB Information Recipient (2017) XD-LAB Information Recipient (2017) | 2008‑08‑08 | | 1.3.6.1.4.1.19376.1.3.10.2.4 | Include |  XD-LAB LegalAuthenticator (2017) XD-LAB LegalAuthenticator (2017) | 2016‑07‑05 | | 1.3.6.1.4.1.19376.1.8.1.4.3 | Include |  CDA authenticator IHE CDA authenticator IHE | 2016‑07‑09 15:03:59 | | 1.3.6.1.4.1.19376.1.3.3.1.6 | Include |  Ordering Provider (2017) Ordering Provider (2017) | 2008‑08‑08 | | 1.3.6.1.4.1.19376.1.8.1.4.1 | Include |  CDA Participant Specimen Collector CDA Participant Specimen Collector | 2016‑06‑13 14:21:13 | | 1.3.6.1.4.1.19376.1.3.10.2.5 | Include |  CDA Participant Pertinent Insurance Information CDA Participant Pertinent Insurance Information | 2017‑11‑13 16:52:30 | | 1.3.6.1.4.1.19376.1.3.3.1.7 | Containment |  Laboratory Performer (2017) Laboratory Performer (2017) | 2008‑08‑08 | | 2.16.840.1.113883.10.12.113 | Include |  CDA componentOf CDA componentOf | 2005‑09‑07 | | 1.3.6.1.4.1.19376.1.8.1.2.1 | Containment |  Clinical Information Section (2.0) Clinical Information Section (2.0) | 2014‑05‑13 14:38:08 | | 1.3.6.1.4.1.19376.1.8.1.2.2 | Containment |  Intraoperative Observation Section (2.0) Intraoperative Observation Section (2.0) | 2014‑05‑13 19:29:16 | | 1.3.6.1.4.1.19376.1.8.1.2.3 | Containment |  Macroscopic Observation Section (2.0) Macroscopic Observation Section (2.0) | 2014‑05‑13 11:57:09 | | 1.3.6.1.4.1.19376.1.8.1.2.4 | Containment |  Microscopic Observation Section (2.0) Microscopic Observation Section (2.0) | 2014‑05‑13 14:25:17 | | 1.3.6.1.4.1.19376.1.3.10.3.1 | Containment |  Additional Specified Observation Section (2.0) Additional Specified Observation Section (2.0) | 2016‑11‑13 14:28:08 | | 1.3.6.1.4.1.19376.1.8.1.2.5 | Containment |  Diagnostic Conclusion Section (2.0) Diagnostic Conclusion Section (2.0) | 2014‑05‑13 19:31:26 | | 1.3.6.1.4.1.19376.1.8.1.2.6 | Containment |  Procedure Steps Section (2.0) Procedure Steps Section (2.0) | 2014‑05‑13 19:33:12 |
|
|
|---|
| Relationship | Specialization: template 2.16.840.1.113883.10.12.1 (2005‑09‑07) |
|---|
| Example | | example for use case #1 | <ClinicalDocument xsi:schemaLocation="urn:hl7-org:v3 infrastructure/cda/CDA_extended.xsd">
<realmCode code="UV"/> <typeId extension="POCD_HD000040" root="2.16.840.1.113883.1.3"/> <templateId root="1.3.6.1.4.1.19376.1.8.1.1.1"/> <id root="1.3.6.1.4.1.19376.1.8.9.1" extension="A7102400008_1" assigningAuthorityName="IHE PaLM Technical Committee"/> <code code="60568-3" codeSystem="2.16.840.1.113883.6.1" displayName="Pathology Synoptic report"/> <title>Anatomic Pathology Structured Report - Breast Biopsy</title> <effectiveTime value="201001041605-0500"/> <confidentialityCode code="N" displayName="normal" codeSystem="2.16.840.1.113883.5.25"/> <languageCode code="en-US"/> <setId root="1.3.6.1.4.1.19376.1.8.9.1" extension="A7102400008" assigningAuthorityName="IHE PaLM Technical Committee"/> <versionNumber value="1"/> <!-- Patient -->
<recordTarget>
<patientRole>
<id extension="0411886319605719371016" root="1.3.6.1.4.1.19376.1.8.9.2"/> <addr use="HP">
<streetAddressLine>39 East Street</streetAddressLine> <postalCode>69499</postalCode> <city>Appleton</city> <state>WI</state> <country>United States</country> </addr> <telecom nullFlavor="NASK"/> <patient>
<name>
<prefix>Miss</prefix> <given>EVE</given> <family qualifier="BR">ONEWOMAN</family> </name> <administrativeGenderCode code="F" codeSystem="2.16.840.1.113883.5.1"/> <birthTime value="19710921"/> </patient> </patientRole> </recordTarget> <!-- one or more author(s) of the report, with authoring time -->
<author>
<templateId root="1.3.6.1.4.1.19376.1.8.1.4.2"/> <time value="20100104131933-0500"/> <assignedAuthor>
<id root="1.3.6.1.4.1.19376.1.8.9.3" extension="801234567897"/> <addr nullFlavor="MSK"/> <telecom value="tel:+33-602030499"/> <assignedPerson>
<name>
<given>Marcel</given> <family>Pathologist</family> <suffix>Ph D</suffix> </name> </assignedPerson> <representedOrganization>
<id root="1.3.6.1.4.1.19376.1.8.9.4" extension="1120456789"/> <name>CANCER INSTITUTE</name> <telecom nullFlavor="MSK"/> <addr nullFlavor="MSK"/> </representedOrganization> </assignedAuthor> </author> <!-- one or more transcriptionists, with transcription time -->
<dataEnterer>
<time value="20100104131720-0500"/> <assignedEntity>
<id root="1.3.6.1.4.1.19376.1.8.9.3" extension="A32"/> <addr nullFlavor="MSK"/> <telecom nullFlavor="MSK"/> <assignedPerson>
<name>
<given>Adeline</given> <family>Medsecret</family> </name> </assignedPerson> </assignedEntity> </dataEnterer> <informant>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.6 'CDA Informant(Body) APSR2' (dynamic), not used in use case #1 -->
</informant> <!-- The unique custodian of this document is the sending pathology lab that will administer it (further updates, deprecation) -->
<custodian>
<assignedCustodian>
<representedCustodianOrganization>
<id root="1.3.6.1.4.1.19376.1.8.9.4" extension="1120456789"/> <name>CANCER INSTITUTE</name> <telecom use="PUB" value="0466666666"/> <addr>
<streetAddressLine>38 Cramberry Street</streetAddressLine> <postalCode>69499</postalCode> <city>Appleton</city> <state>WI</state> </addr> </representedCustodianOrganization> </assignedCustodian> </custodian> <!-- One or more additional intended recipients (other than the ordering physician) -->
<informationRecipient>
<templateId root="1.3.6.1.4.1.19376.1.3.3.1.4"/> <intendedRecipient>
<id root="1.3.6.1.4.1.19376.1.8.9.3" extension="987"/> <addr>
<streetAddressLine>1600 Clifton Road</streetAddressLine> <city>Atlanta</city> <state>GA</state> <postalCode>30333</postalCode> </addr> <telecom value="tel:404-639-3535"/> <informationRecipient>
<name>
<family>WOULDLIKETOKNOW</family> <given>Thomas</given> </name> </informationRecipient> </intendedRecipient> </informationRecipient> <!-- The unique legal authenticator: The person assuming the final responsibility of the report and signing it -->
<legalAuthenticator>
<time value="20100104152503-0500"/> <signatureCode code="S"/> <assignedEntity>
<id root="1.3.6.1.4.1.19376.1.8.9.3" extension="801234567897"/> <assignedPerson>
<name>
<given>Marcel</given> <family>Pathologist</family> </name> </assignedPerson> </assignedEntity> </legalAuthenticator> <!-- Zero or more additional content validator(s): pathologists having validated some part of the report -->
<authenticator>
<templateId root="1.3.6.1.4.1.19376.1.8.1.4.3"/> <time value="20100104142503-0500"/> <signatureCode code="S"/> <assignedEntity>
<id root="1.3.6.1.4.1.19376.1.8.9.3" extension="801234567898"/> <addr nullFlavor="MSK"/> <telecom nullFlavor="MSK"/> <assignedPerson>
<name>
<given>Jonas</given> <family>Jones</family> <prefix>MD</prefix> </name> </assignedPerson> </assignedEntity> </authenticator> <!-- The ordering physician -->
<participant typeCode="REF">
<templateId root="1.3.6.1.4.1.19376.1.3.3.1.6"/> <time>
<high value="20091231"/> </time> <associatedEntity classCode="PROV">
<id root="1.3.6.1.4.1.19376.1.8.9.3" extension="801234567892"/> <addr nullFlavor="NASK"/> <telecom value="tel:0147150000" use="EC"/> <associatedPerson>
<name>
<prefix>Doctor</prefix> <given>Eva</given> <family>Surgeon</family> <suffix>Ph D</suffix> </name> </associatedPerson> </associatedEntity> </participant> <!-- include template 1.3.6.1.4.1.19376.1.8.1.4.1 'CDA participant specimen collector' (dynamic) 0..* R, not used in use case #1 -->
<!-- include template 1.3.6.1.4.1.19376.1.3.10.2.5 'CDA participant pertinent insurance information' (dynamic) 0..1 R, not used in use case #1 -->
<!-- Identification of the order, extension is Order-ID -->
<inFulfillmentOf>
<order>
<id root="1.3.6.1.4.1.19376.1.8.9.8" extension="12345"/> </order> </inFulfillmentOf> <!-- Documented act(s): The pathology examination procedure, extension is Accession number -->
<documentationOf>
<serviceEvent>
<id root="1.3.6.1.4.1.19376.1.8.9.9" extension="A7102400008"/> <code code="371528001" displayName="Pathology report (record artifact)" codeSystem="2.16.840.1.113883.6.96" codeSystemName="SNOMED CT"/> <lab:statusCode code="completed"/> <effectiveTime>
<!-- Start: Date&time of reception of this order and the attached specimens -->
<low value="200912300922-0500"/> <!-- End -->
<high value="201001041605-0500"/> </effectiveTime> <!-- Performing laboratory -->
<performer typeCode="PRF">
<templateId root="1.3.6.1.4.1.19376.1.3.3.1.7"/> <time>
<high value="201001041605-0500"/> </time> <assignedEntity>
<id root="1.3.6.1.4.1.19376.1.8.9.3" extension="801234567897"/> <representedOrganization>
<id root="1.3.6.1.4.1.19376.1.8.9.4" extension="1120456789"/> <name>CANCER INSTITUTE</name> <telecom nullFlavor="MSK"/> <addr nullFlavor="MSK"/> </representedOrganization> </assignedEntity> </performer> </serviceEvent> </documentationOf> <!-- include template 1.3.6.1.4.1.19376.1.3.1.9999.10.9.16 'RelatedDocument Parent Document' (dynamic) 0..1 R, not used in use case #1 -->
<!-- Patient encounter: The patient stay in the hospital where the surgery was performed -->
<componentOf>
<encompassingEncounter>
<id root="1.3.6.1.4.1.19376.1.8.9.7" extension="234567890"/> <code code="ACUTE" displayName="inpatient acute"/> <effectiveTime>
<high value="2201001040735-0500"/> </effectiveTime> <location typeCode="LOC">
<healthCareFacility classCode="SDLOC">
<id root="1.3.6.1.4.1.19376.1.8.9.4" extension="11223344"/> <serviceProviderOrganization classCode="ORG" determinerCode="INSTANCE">
<name>Surgery theater</name> <asOrganizationPartOf>
<wholeOrganization>
<name>CANCER INSTITUTE</name> </wholeOrganization> </asOrganizationPartOf> </serviceProviderOrganization> </healthCareFacility> </location> </encompassingEncounter> </componentOf> <!-- Structured body -->
<component typeCode="COMP" contextConductionInd="true">
<structuredBody classCode="DOCBODY" moodCode="EVN">
<component typeCode="COMP" contextConductionInd="true">
<!-- template 1.3.6.1.4.1.19376.1.8.1.2.1 'Clinical Information Section' (2014-05-13T14:38:08) -->
</component> <component typeCode="COMP" contextConductionInd="true">
<!-- template 1.3.6.1.4.1.19376.1.8.1.2.2 'Intraoperative Observation Section' (2014-05-13T19:29:16) -->
</component> <component typeCode="COMP" contextConductionInd="true">
<!-- template 1.3.6.1.4.1.19376.1.8.1.2.3 'Macroscopic Observation Section' (2014-05-13T11:57:09) -->
</component> <component typeCode="COMP" contextConductionInd="true">
<!-- template 1.3.6.1.4.1.19376.1.8.1.2.4 'Microscopic Observation Section' (2014-05-13T14:25:17) -->
</component> <component typeCode="COMP" contextConductionInd="true">
<!-- template 1.3.6.1.4.1.19376.1.3.10.3.1 'Additionally Specified Observation Section' (2016-11-13T14:28:08) -->
</component> <component typeCode="COMP" contextConductionInd="true">
<!-- template 1.3.6.1.4.1.19376.1.8.1.2.5 'Diagnostic Conclusion Section' (2014-05-13T19:31:26) -->
</component> <component typeCode="COMP" contextConductionInd="true">
<!-- template 1.3.6.1.4.1.19376.1.8.1.2.6 'Procedure Steps Section' (2014-05-13T19:33:12) -->
</component> </structuredBody> </component></ClinicalDocument> |
|
| Item | DT | Card | Conf | Description | Label |
|---|
| | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  | @classCode
|
| cs | 1 … 1 | F | DOCCLIN |  | @moodCode
|
| cs | 1 … 1 | F | EVN |  | hl7:templateId
|
| II | 1 … 1 | M | This element is identifying the set of constraints applied to the CDA R2 standard by this IHE specification of a AP report. The following templateId SHALL be present and valued as follows to indicate compliance with the APSR 2.0 content module specification.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @root
|
| uid | 1 … 1 | F | 1.3.6.1.4.1.19376.1.8.1.1.1 |  | hl7:realmCode
|
| CS (extensible) | 1 … 1 | M | This element SHALL be present and is valued from the RealmOfUse [2.16.840.1.113883.1.11.11050] subset, within the VocabularyDomainQualifier value set. In the international context of this profile used as it is without any further extension, the realm code SHALL be <realmCode code="UV"/> (universal). Whenever a national extension has been defined and is used, the realm code SHALL identify this national extension. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  | hl7:typeId
|
| II | 1 … 1 | M | This element is a technology-neutral explicit reference to the standard CDA R2. It SHALL be present and valued as follows:
ClinicalDocument/typeId@root = "2.16.840.1.113883.1.3" (which is the OID for HL7 Registered models);
ClinicalDocument.typeId@extension = "POCD_HD000040" (which is the unique identifier for the CDA, Release Two Hierarchical Description).
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @root
|
| uid | 1 … 1 | F | 2.16.840.1.113883.1.3 |  |  | @extension
|
| st | 1 … 1 | F | POCD_HD000040 |  | hl7:id
|
| II | 1 … 1 | M | ClinicalDocument/Id SHALL be present. It represents the unique instance identifier of the clinical document. The combination of the root and extension attributes SHALL provide a globally unique identifier, in accordance with CDA R2, without further constraints.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @root
|
| uid | 1 … 1 | R | Here the OID for PAT exemplary instances, in practice the OID of the LIS |  |  | @extension
|
| st | 1 … 1 | R | Here a hypothetical document ID, most often derived from the accession number
| | | Constraint | A report may have several successive revisions over time, in case corrections or complements are provided by the custodian after the initial release of the report.
The unique id of the current revision of the report is carried by the
id element, and is composed of
- id@root, which SHALL be an OID,
- and optionally id@extension, which can be any string so that the concatenation of the two attributes root and extension provide a globally unique id, which identifies this release of the report.
| | | Example | Report ID from use case #1 <id root="1.3.6.1.4.1.19376.1.8.9.1" extension="A7102400008_1" assigningAuthorityName="IHE PaLM Technical Committee"/> |  | hl7:code
|
| CE (required) | 1 … 1 | M | ClinicalDocument/code SHALL be present. The document type of this content module is always
<code code="60568-3"
codeSystem="2.16.840.1.113883.6.1"
displayName="Pathology Synoptic report"
codeSystemName="LOINC"/>
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @code
|
| CONF | 1 … 1 | F | 60568-3 |  |  | @codeSystem
|
| 1 … 1 | F | 2.16.840.1.113883.6.1 (Logical Observation Identifier Names and Codes) |  |  | @codeSystemName
|
| 1 … 1 | F | LOINC |  |  | @displayName
|
| 1 … 1 | F | Pathology Synoptic report |  | hl7:title
|
| ST | 1 … 1 | M | The APSR <title> SHALL be present. It is the local translation of the code@displayName.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | CONF | | element content shall be "Anatomic Pathology Structured Report" |
| | | Example | Report title from use case #1 <title>ANATOMIC PATHOLOGY REPORT - BREAST BIOPSY</title> |  | hl7:effectiveTime
|
| TS | 1 … 1 | M | ClinicalDocument/effectiveTime SHALL be present. It contains the creation date & time of the laboratory report as an electronic document. In case this is a new revision replacing a previous version (identified in parentDocument), this is the date & time of the new revision.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  | hl7:confidentialityCode
|
| CE (required) | 1 … 1 | M | ClinicalDocument/confidentialityCode SHALL be present in accordance with the HL7 CDA R2 standard.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | CONF | | The value of @code shall be drawn from value set 2.16.840.1.113883.1.11.16926 HL7 BasicConfidentialityKind (2014‑06‑09) |
|  | hl7:languageCode
|
| CS (required) | 1 … 1 | M | ClinicalDocument/languageCode SHALL be present in accordance with the HL7 CDA R2 standard.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | CONF | | The value of @code shall be drawn from value set 2.16.840.1.113883.1.11.11526 HumanLanguage (2014‑03‑26) |
|  | hl7:setId
|
| II | 1 … 1 | M | ClinicalDocument/setId SHALL be present to enable further updates of the clinical document. It is an identifier that is common across all revisions of this AP report.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @root
|
| uid | 1 … 1 | R | |  |  | @extension
|
| st | 1 … 1 | R | | | | Constraint | A report may have several successive revisions over time, in case corrections or complements are provided by the custodian after the initial release of the report.
The setId element provides a globally unique identifier that is common across all successive revisions of the report. This identifier is similarly composed of setId@root, which SHALL be an OID, and optionally setId@extension. | | | Example | Report set ID from use case #1 <id root="1.3.6.1.4.1.19376.1.8.9.1" extension="A7102400008" assigningAuthorityName="IHE PaLM Technical Committee"/> |  | hl7:versionNumber
|
| INT | 0 … 1 | R | ClinicalDocument/versionNumber MAY be present. As requested by the CDA standard, it is an integer value used as versioning.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @value
|
| int | 1 … 1 | R | | | | Constraint | A report may have several successive revisions over time, in case corrections or complements are provided by the custodian after the initial release of the report.
The version number of the current revision of the report is a positive integer (1, 2 …) provided in the versionNumber element. | | | Example | Report version number for use case #1 <versionNumber value="1"/> | | Included | 1 … 1 | M | from 1.3.6.1.4.1.19376.1.3.3.1.1 Human Patient (2017‑06‑07)
The Patient.
The anatomic pathology report is related to ONE SINGLE patient.
-
A patient SHALL be identified with at least one unique patientRole/Id.
-
The patient address and telecom SHALL be provided (or null flavored).
-
The patient identity SHALL provide AT LEASTthe patient full name, sex and date/time of birth.
|  | hl7:recordTarget
|
| | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | hl7:patientRole
|
| | 1 … 1 | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | II | 1 … * | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | AD | 1 … * | | All persons (including the patient) and organizations mentioned in the document SHALL provide elements name, addr and telecom. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | TEL | 1 … * | | All persons (including the patient) and organizations mentioned in the document SHALL provide elements name, addr and telecom. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 1 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | II | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | PN | 1 … * | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  |  | hl7:administrativeGenderCode
|
| CE | 1 … 1 | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | TS | 1 … 1 | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | Included | 1 … * | M | from 1.3.6.1.4.1.19376.1.8.1.4.2 CDA author IHE (2016‑06‑21 14:02:11)
The Author Content Module represents an author of the report. This element is repeatable. The sub-element author/time carries the date/time of the authoring action.
At least one ClinicalDocument/author SHALL be present with a time in accordance with the HL7 CDA R2 standard and further constrained by this specification to require the presence of name, addr and telecom. The author/time element carries the date&time the AP report was produced. The AP report can be authored by a software system or by a person or by both.
Source: PaLM Suppl.APSR 2.0‑3: 6.3.6.2
|  | hl7:author
|
| | 1 … * | M | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author |  |  | @typeCode
|
| cs | 1 … 1 | F | AUT | | | Example | author is a person <author typeCode="AUT" contextControlCode="OP">
<time value="201306101654"/> <assignedAuthor classCode="ASSIGNED">
<!-- ... -->
</assignedAuthor></author> |  |  | hl7:templateId
|
| | 1 … 1 | M | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | uid | 1 … 1 | F | 1.3.6.1.4.1.19376.1.8.1.4.2 |  |  | hl7:time
|
| TS | 1 … 1 | M | The authoring time is the date & time that this author contributed to the document. It SHALL be provided. | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author |  |  | hl7:assignedAuthor
|
| | 0 … 1 | C | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | cs | 0 … 1 | F | ASSIGNED | | II | 1 … * | M | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | AD | 1 … * | M | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | TEL | 1 … * | M | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | Choice | 1 … 1 | | The author is either an assigned person or an authoring device.
Elements to choose from:- hl7:assignedPerson
- hl7:assignedAuthoringDevice
| | | 0 … 1 | C | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | Included | 0 … * | | from 2.16.840.1.113883.10.12.152 CDA Person (2005‑09‑07)
The name(s) SHALL be given. | | | 0 … 1 | F | PSN | | | 0 … 1 | F | INSTANCE | | PN | 0 … * | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author |  |  |  |  | hl7:assignedAuthoringDevice
|
| | 0 … 1 | C | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | cs | 0 … 1 | F | DEV | | cs | 0 … 1 | F | INSTANCE |  |  |  |  |  | hl7:manufacturerModelName
|
| SC | 0 … 1 | R | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | SC | 0 … 1 | R | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | CE | 0 … 1 | R | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author |  |  |  | hl7:representedOrganization
|
| | 0 … 1 | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | | Example | represented organization for author as a device <representedOrganization classCode="ORG" determinerCode="INSTANCE">
<name>
<!-- ... -->
</name></representedOrganization> | | Included | 0 … 1 | | from 2.16.840.1.113883.10.12.151 CDA Organization (2005‑09‑07)
The identifier(s) SHOULD, the name SHALL, the telecom(s) and the address(es) MAY be given. | | | 0 … 1 | F | ORG | | | 0 … 1 | F | INSTANCE | | II | 0 … 1 | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | ON | 0 … 1 | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | TEL | 0 … 1 | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | AD | 0 … 1 | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author |  |  |  |  | hl7:standardIndustryClassCode
|
| CE | 0 … 1 | | SHALL be chosen from domain OrganizationIndustryClass | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | | 0 … 1 | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | | 0 … 1 | F | PART | | II | 0 … * | R | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | CE | 0 … 1 | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | CONF | 0 … 1 | F | 2.16.840.1.113883.5.111 (Role Code) | | CS | 0 … 1 | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | | CONF | | The value of @code shall be drawn from value set 2.16.840.1.113883.1.11.15999 RoleStatus (DYNAMIC) |
| | IVL_TS | 0 … 1 | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | | 0 … 1 | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | | 0 … 1 | F | ORG | | | 0 … 1 | F | INSTANCE | | II | 0 … * | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | ON | 0 … * | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | TEL | 0 … * | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | AD | 0 … * | | | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author |  |  |  |  |  |  | hl7:standardIndustryClassCode
|
| CE | 0 … 1 | | SHALL be chosen from domain OrganizationIndustryClass | PaLM Suppl.APSR 2.0‑3:6.3.6.2 Author | | Included | 0 … * | R | from 2.16.840.1.113883.10.12.103 CDA dataEnterer (2005‑09‑07)
Transcriptionist
|  | hl7:dataEnterer
|
| | 0 … * | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @typeCode
|
| | 0 … 1 | F | ENT |  |  | @contextControlCode
|
| | 0 … 1 | F | OP |  |  | hl7:time
|
| TS | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | hl7:assignedEntity
|
| | 1 … 1 | | Contains 2.16.840.1.113883.10.12.153 CDA AssignedEntity (DYNAMIC) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  | hl7:informant
|
| | 0 … * | R | Zero or more informant MAY be mentioned in the header of the report. An informant is either an assignedEntity (a professional participating to the healthcare process, and who was assigned a defined role in that process) or a relatedEntity (a person who knows the patient and has provided relevant information concerning the patient). Hence the condition is either assignedEntity is present or relatedEntity is present. These two elements are defined in the content module “Informant”.
Source: PaLM Suppl. APSR 2.0-3: 6.3.6.5
Contains 1.3.6.1.4.1.19376.1.8.1.4.6 CDA Informant(Header&Body) APSR2 (2016‑07‑08 11:22:58) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  | where [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.6']] |
| | | Included | 1 … 1 | M | from 2.16.840.1.113883.10.12.104 CDA custodian (2005‑09‑07)
ClinicalDocument/custodian SHALL be present with an id in accordance with the HL7 CDA R2 standard and further constrained by this specification to require the presence of name, addr and telecom. It represents the organization that is in charge of maintaining the AP report.
|  | hl7:custodian
|
| | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @typeCode
|
| | 0 … 1 | F | CST |  |  | hl7:assignedCustodian
|
| | 1 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 0 … 1 | F | ASSIGNED |  |  |  | hl7:representedCustodianOrganization
|
| | 1 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 0 … 1 | F | ORG | | | 0 … 1 | F | INSTANCE | | II | 1 … * | M | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | ON | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | TEL | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | AD | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | Included | 0 … * | R | from 1.3.6.1.4.1.19376.1.3.3.1.4 XD-LAB Information Recipient (2008‑08‑08)
The Intended Recipient Content Module represents a healthcare provider,
other than the ordering physician, expecting to receive a copy of the report. This repeatable element informationRecipient of the CDA header is used to list the intended recipients who were known at the time the report was created and issued.
Source: PaLM TF-3: 6.3.2.14
|  | hl7:informationRecipient
|
| | 0 … * | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | hl7:templateId
|
| II | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | uid | 1 … 1 | F | 1.3.6.1.4.1.19376.1.3.3.1.4 |  |  | hl7:intendedRecipient
|
| | 1 … 1 | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | II | 0 … * | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | AD | 1 … * | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | TEL | 1 … * | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | hl7:informationRecipient
|
| | 0 … 1 | | Contains 1.3.6.1.4.1.19376.1.3.10.9.18 PlayingEntity or person with Name (DYNAMIC) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | hl7:receivedOrganization
|
| | 0 … 1 | | Contains 1.3.6.1.4.1.19376.1.3.10.9.13 Organization with Name, Addr, Telecom (DYNAMIC) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | Included | 1 … 1 | M | from 1.3.6.1.4.1.19376.1.3.10.2.4 XD-LAB LegalAuthenticator (2016‑07‑05)
The Legal authenticator Content Module describes a pathologist having verified the content of the report, using the element legalAuthenticator.
The report SHALL have one legal Authenticator
Source: PaLM TF-3: 6.3.2.15
|  | hl7:legalAuthenticator
|
| | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | hl7:time
|
| TS | 1 … 1 | R | The sub-element time carries the date&time this legal authentication took place. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | hl7:signatureCode
|
| CS | 1 … 1 | R | The sub-element signatureCode carries the “signed” (S) status | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | CONF | 0 … 1 | F | S |  |  | hl7:assignedEntity
|
| | 1 … 1 | R | All persons (including the patient) and organizations mentioned in the document SHALL provide elements name, addr and telecom. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | AD | 1 … * | R | Constrained by this specification to require the presence of name, addr and telecom. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | TEL | 1 … * | R | Constrained by this specification to require the presence of name, addr and telecom. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 0 … 1 | | All persons (including the patient) and organizations mentioned in the document SHALL provide elements name, addr and telecom.
Contains 1.3.6.1.4.1.19376.1.3.10.9.18 PlayingEntity or person with Name (DYNAMIC) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | hl7:representedOrganization
|
| | 0 … 1 | | All persons (including the patient) and organizations mentioned in the document SHALL provide elements name, addr and telecom.
Contains 1.3.6.1.4.1.19376.1.3.10.9.13 Organization with Name, Addr, Telecom (DYNAMIC) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | Included | 0 … * | R | from 1.3.6.1.4.1.19376.1.8.1.4.3 CDA authenticator IHE (2016‑07‑09 15:03:59)
The Content validator Content Module describes a pathologist having verified the content of the report, using the element authenticator. This element authenticator is used when the pathologist having verified the content of the report is distinct from the pathologist assuming the legal responsibility for this report, described in the legalAuthenticator element.
The report MAY have zero or more Content Validators.
Source: PaLM Suppl. APSR 2.0-3: 6.3.6.3
|  | hl7:authenticator
|
| | 0 … * | R | | PaLM Suppl. APSR 2.0‑3: 6.3.6.3 Content validator |  |  | @typeCode
|
| cs | 1 … 1 | F | AUTHEN |  |  | hl7:templateId
|
| | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.6.3 Content validator | | uid | 1 … 1 | F | 1.3.6.1.4.1.19376.1.8.1.4.3 |  |  | hl7:time
|
| TS | 1 … 1 | R | Time of validation | PaLM Suppl. APSR 2.0‑3: 6.3.6.3 Content validator |  |  | hl7:assignedEntity
|
| | 0 … 1 | C | AssignedPerson SHALL be given with name, representedOrganization MAY be given.
Contains 2.16.840.1.113883.10.12.153 CDA AssignedEntity (2005‑09‑07) | PaLM Suppl. APSR 2.0‑3: 6.3.6.3 Content validator | | Included | 1 … 1 | R | from 1.3.6.1.4.1.19376.1.3.3.1.6 Ordering Provider (2008‑08‑08)
The Ordering Provider Content Module represents the physician who has submitted the specimen examination order to the anatomic pathology laboratory. As specified in PaLM TF-3, this physician is represented in the CDA header as a participant element with the typeCode attribute valued “REF”. The sub-element participant/time carries the date/time of issuance of the
order.
Source: PaLM TF-3: 6.3.2.17
|  | hl7:participant
|
| | 1 … 1 | R | Referral Ordering Physician | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @typeCode
|
| cs | 1 … 1 | F | REF |  |  | hl7:templateId
|
| II | 1 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | uid | 1 … 1 | F | 1.3.6.1.4.1.19376.1.3.3.1.6 |  |  | hl7:time
|
| IVL_TS | 1 … 1 | R | This element represents the date and time the order was placed. Time MAY be present. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | hl7:associatedEntity
|
| | 1 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | AD | 1 … * | R | The address of this person (referral ordering physician) SHALL be present. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | TEL.AT | 1 … * | R | The telecom of this person (referral ordering physician) SHALL be present. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | Schematron assert | role |  error error | | | | test | not(hl7:assignedPerson) or hl7:assignedPerson/hl7:name | | | | Message | The <name> sub-element SHALL be present when <assignedPerson> present. | | | | 0 … 1 | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | Included | 0 … * | R | from 1.3.6.1.4.1.19376.1.8.1.4.1 CDA Participant Specimen Collector (2016‑06‑13 14:21:13)
The Specimen Collector Content Module is only used in case a specimen
provided as input to the AP act documented in this report, was collected by a different party than the ordering physician. In that case, this specimen collector is represented in the CDA header as a participant element with the typeCode attribute valued “DIST” and the sub-element participant/time carries the time period of the specimen collection.
Source: PAT TF-3: 6.2.6.1
|  | hl7:participant
|
| | 0 … * | R | The Specimen Collector Content Module is only used in case a specimen provided as input to the AP act documented in this report, was collected by a different party than the ordering physician. In that case, this specimen collector is represented in the CDA header as a participant element with the typeCode attribute valued “DIST” and the sub-element participant/time carries the time period of the specimen collection.
| PaLM Suppl. APSR 2.0‑3:6.3.6.1 Specimen collector |  |  | @typeCode
|
| cs | 1 … 1 | F | DIST |  |  | hl7:templateID
|
| II | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3:6.3.6.1 Specimen collector | | uid | 1 … 1 | F | 1.3.6.1.4.1.19376.1.8.1.4.1 |  |  | hl7:time
|
| IVL_TS | 1 … 1 | M | Specimen collection time
The specimen collection time is an interval, which may be reduced to a point in time (see usage of data type IVL_TS).
| PaLM Suppl. APSR 2.0‑3:6.3.6.1 Specimen collector |  |  | hl7:associatedEntity
|
| | 0 … 1 | R | At least one of the two elements
associatedPerson
and
scopingOrganization
must be present. Both may be present.
| PaLM Suppl. APSR 2.0‑3:6.3.6.1 Specimen collector | | cs | 1 … 1 | F | PROV | | II | 1 … * | R | | PaLM Suppl. APSR 2.0‑3:6.3.6.1 Specimen collector | | AD | 1 … * | R | | PaLM Suppl. APSR 2.0‑3:6.3.6.1 Specimen collector | | TEL.AT | 1 … * | R | | PaLM Suppl. APSR 2.0‑3:6.3.6.1 Specimen collector | | | 0 … * | C | Person who collected the specimen.
Only full name(s) SHALL be given.
Contains 2.16.840.1.113883.10.12.152 CDA Person (2005‑09‑07) | PaLM Suppl. APSR 2.0‑3:6.3.6.1 Specimen collector | | | 0 … 1 | C | Organization taking care for specimen collection.
Identifiers, name, telecom, and address SHOULD be given.
Contains 2.16.840.1.113883.10.12.151 CDA Organization (2005‑09‑07) | PaLM Suppl. APSR 2.0‑3:6.3.6.1 Specimen collector | | Included | 0 … 1 | R | from 1.3.6.1.4.1.19376.1.3.10.2.5 CDA Participant Pertinent Insurance Information (2017‑11‑13 16:52:30)
Key insurance information of the patient |  | hl7:participant
|
| | 0 … 1 | R | Insurance information of the patient in context for reporting to cancer registries (in Germany) | PaLM Suppl. 2.0‑3:6.3.6.13 |  |  | @typeCode
|
| cs | 1 … 1 | F | HLD |  |  | hl7:templateId
|
| II | 1 … * | M | | PaLM Suppl. 2.0‑3:6.3.6.13 | | uid | 1 … 1 | F | 1.3.6.1.4.1.19376.1.3.10.2.5 |  |  | hl7:time
|
| IVL_TS | 0 … 1 | R | time shows the end of the current insurance period, e.g. end of the quartal | PaLM Suppl. 2.0‑3:6.3.6.13 | | | Example | <time>
<high value="20171231"/></time> |  |  | hl7:associatedEntity
|
| | 1 … 1 | M | Data of the insured person | PaLM Suppl. 2.0‑3:6.3.6.13 | | cs | 1 … 1 | F | POLHOLD | | II | 0 … * | R | ID(s) of the insured person (patient), e.g. ID of the insured, ID of the health card, etc. | PaLM Suppl. 2.0‑3:6.3.6.13 | | CE | 0 … 1 | R | status of the insured person | PaLM Suppl. 2.0‑3:6.3.6.13 | | CONF | 0 … 1 | F | 2.16.840.1.113883.5.111 (Role Code) | | | Example | <code code="SELF" codeSystem="2.16.840.1.113883.5.111" displayName="self">
<translation code="1" codeSystem="2.16.840.1.113883.3.7.1.1" displayName="member"/></code> | | CV | 0 … 1 | R | further codes of the status of the insured person,
e.g. for Germany from value set S_KBV_VERSICHERTENSTATUS
1.2.276.0.76.11.162 | PaLM Suppl. 2.0‑3:6.3.6.13 | | AD | 0 … 1 | R | | PaLM Suppl. 2.0‑3:6.3.6.13 | | TEL | 0 … * | R | | PaLM Suppl. 2.0‑3:6.3.6.13 | | | 0 … 1 | R | Data of the insured person, which may be different from the patient.
Contains 2.16.840.1.113883.10.12.152 CDA Person (2005‑09‑07) | PaLM Suppl. 2.0‑3:6.3.6.13 | | | 1 … 1 | R | Data of the Insurance company, including the ID, the address data and the name.
In Germany the ID is formed by the ID itself (@extension = so-called IKNR) and the OID for IKNR (@root="1.2.276.0.76.4.5") in Germany.
Contains 2.16.840.1.113883.10.12.151 CDA Organization (2005‑09‑07) | PaLM Suppl. 2.0‑3:6.3.6.13 |  | hl7:inFulfillmentOf
|
| | 0 … 1 | R | The inFulfillmentOf/order element MAY be present. It represents the Placer Order or the Placer Group that was fulfilled, the Id of which is carried by inFulfillmentOf/order/id.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @typeCode
|
| cs | 1 … 1 | F | FLFS |  |  | hl7:order
|
| | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | cs | 1 … 1 | F | ACT | | cs | 1 … 1 | F | RQO | | II | 1 … * | R | Placer order group ID or Placer order ID
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  | hl7:documentationOf
|
| | 1 … 1 | M | Documented act. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @typeCode
|
| cs | 1 … 1 | F | DOC |  |  | hl7:serviceEvent
|
| | 1 … 1 | M | The AP report is documenting a service (documentationOf/serviceEvent) performed by a surgical pathology laboratory. The Laboratory Performer Content Module represents this laboratory, and is fully described in the sub-element
documentationOf/serviceEvent/performer.
In case more than one laboratory contributed to a service, only the primary laboratory is in the CDA header, attached to the serviceEvent element, and the other (secondary) laboratories are described only in the sections of the report that they contributed to, in the body of the report.
Source: PaLM TF3: 6.3.2.19
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | cs | 1 … 1 | R | | | cs | 1 … 1 | R | | | II | 1 … * | M | ID of the Act, i.e. Accession number | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | CE (extensible) | 0 … 1 | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | CONF | | @code shall be "PATREPE" | | @codeSystem shall be "2.16.840.1.113883.5.4" | | @codeSystemName shall be "HL7 ActCode" | | @displayName shall be "pathology report entry task" | | or | | @code shall be "371528001" | | @codeSystem shall be "2.16.840.1.113883.6.96" | | @codeSystemName shall be "SCT" | | @displayName shall be "Pathology report (record artifact)" |
| | IVL_TS | 0 … 1 | R | Use of sub element documentationOf/serviceEvent/effectiveTime to document the time boundaries of events in the document is appropriate.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | CS (required) | 0 … 1 | R |
The statusCode below documentationOf/serviceEvent is an extension to the CDA R2 standard, added by PaLM TF-3 to distinguish a preliminary report (statusCode@code="active") from a final report (statusCode@code="completed").
The statusCode sub element is further described in section A.3 of PaLM TF-3. This sub-element is required. When it is not there, the documented Act is assumed to be completed and the report is assumed to be a final report.
This extension to the standard is protected by a dedicated namespace associated in the ClinicalDocument element to the prefix lab:
<Clinical Document xmlns:lab="urn:oid:1.3.6.1.4.1.19376.1.3.2" … >
Source: PaLM TF3: 6.3.2.19
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | Constraint | The statusCode@code="completed" is only applicable, if ALL content modules of the Clinical Document have the statusCode@code="completed", too, or have the statusCode@code="aborted".
| | | CONF | | The value of @code shall be drawn from value set 1.3.6.1.4.1.19376.1.3.11.4 ActStatusActiveCompleted (2008‑08‑08) |
| | | Schematron assert | role |  error error | | | | test | hl7:serviceEvent/lab:statusCode[@code='completed'] | | | | Message | Status code of all Content Modules SHALL be "complete" or "aborted" | | | | 0 … * | R | Contains 1.3.6.1.4.1.19376.1.3.3.1.7 Laboratory Performer (2008‑08‑08) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | where [hl7:templateId [@root='1.3.6.1.4.1.19376.1.3.3.1.7']] |
| |  | hl7:relatedDocument
|
| | 0 … 1 | R | ClinicalDocument/relatedDocument/parentDocument
This element SHALL be present in case of an update replacement of a previous report. In this case relatedDocument@typeCode attribute SHALL be valued "RPLC", the new report replacing the parent one.
Note 1: A non-final AP structured report published in an XDS infrastructure will likely be replaced afterwards by the final report. When this event occurs, the Content Creator Actor SHALL apply the following rules:
- ClinicalDocument/setId SHALL have the same value in the new report as in the replaced report.
- ClinicalDocument/versionNumber SHALL be incremented in the replacing report (i.e., the final one).
- ClinicalDocument/relatedDocument@typeCode attribute SHALL be valued ”RPLC”
- ClinicalDocument/relatedDocument/parentDocument/id in the new report SHALL be equal to ClinicalDocument/ id of the replaced document.
The Document Source Actor SHALL apply the following rules on XDSDocumentEntry metadata:
- The final report SHALL be associated with the previously published one, using RPLC relationship and the previous report SHALL be “Deprecated” as described in ITI TF-2:4.1.6.1.
Note 2: A non-final report can also be replaced by a more recent, albeit still non-final report. The rules above also apply in this case.
Note 3: A final report can also be replaced by a corrective final report. The rules above also apply in this case. | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @typeCode
|
| cs | 1 … 1 | F | RPLC | | | relatedDocument@typeCode attribute SHALL be valued "RPLC"
|  |  | hl7:parentDocument
|
| ANY | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | II | 1 … 1 | M | SHALL be equal to ClinicalDocument/ id of the replaced document.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | II | 1 … 1 | M | SHALL have the same value in the new report as in the replaced report.
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | INT | 0 … 1 | R | SHALL have the same value as in the replaced report (when provided there).
| PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | Included | 0 … 1 | R | from 2.16.840.1.113883.10.12.113 CDA componentOf (2005‑09‑07)
The ClinicalDocument/componentOf/encompassingEncounter element MAY be present.
It describes the encounter during which the reported AP observations were ordered. When present the encounter SHALL:
- be identified with an id element: encompassingEncounter/id
- The encounter SHALL have an effective time that represents the time interval (possibly still running, e.g., an inpatient current stay) of the encounter or a point in time at which the encounter took place (e.g., an outpatient consultation): encompassingEncounter/ effectiveTime
The encounter MAY provide any number of encounter participants (encompassingEncounter/encounterParticipant/assignedEntity). When present, encounter participants SHALL be in accordance with the HL7 CDA R2 standard with a time and further constrained by this specification to require the presence of name, addr and telecom. Additionally, the encounter participant SHALL have a typeCode with one the values selected from the x_EncounterParticipant domain: The encounter MAY precise the patient location during this encounter. This is the healthcare facility in which the patient was located when the reported AP observations were ordered: encompassingEncounter/location/healthCareFacility. This healthcare facility can be represented as a physical place (e.g., room, floor, building, office) or as an organization (e.g., service, department, team) or both: healthCareFacility/location, healthCareFacility/serviceProviderOrganization. |  | hl7:componentOf
|
| | 0 … 1 | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @typeCode
|
| | 0 … 1 | F | COMP |  |  | hl7:encompassingEncounter
|
| | 1 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 0 … 1 | F | ENC | | | 0 … 1 | F | EVN | | II | 0 … * | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | CE | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | CONF | | The value of @code shall be drawn from value set 2.16.840.1.113883.1.11.13955 ActEncounterCode (DYNAMIC) |
| | IVL_TS | 1 … 1 | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | hl7:dischargeDispositionCode
|
| CE | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | CONF | | shall be drawn from concept domain "EncounterDischargeDisposition" |
| | | 0 … 1 | | Contains 2.16.840.1.113883.10.12.153 CDA AssignedEntity (DYNAMIC) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 0 … 1 | F | RESP | | | 0 … * | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | cs | 1 … 1 | R | | | | CONF | | The value of @typeCode shall be drawn from value set 2.16.840.1.113883.1.11.19600 x_EncounterParticipant (DYNAMIC) |
| | IVL_TS | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 1 … 1 | | Contains 2.16.840.1.113883.10.12.153 CDA AssignedEntity (DYNAMIC) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 0 … 1 | F | LOC | | | 1 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | 0 … 1 | F | SDLOC | | II | 0 … * | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | CE | 0 … 1 | | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | | CONF | | The value of @code shall be drawn from value set 2.16.840.1.113883.1.11.17660 ServiceDeliveryLocationRoleType (DYNAMIC) |
| | | 0 … 1 | | Contains 2.16.840.1.113883.10.12.317 CDA Place (DYNAMIC) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  |  |  | hl7:serviceProviderOrganization
|
| | 0 … 1 | | Contains 2.16.840.1.113883.10.12.151 CDA Organization (DYNAMIC) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  | hl7:component
|
| | 1 … 1 | R | Body of the CDA Clinical document | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP |  |  | @contextConductionInd
|
| bl | 1 … 1 | F | true |  |  | hl7:structuredBody
|
| | 1 … 1 | R | | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module | | cs | 1 … 1 | F | DOCBODY | | cs | 1 … 1 | F | EVN | | | 0 … 1 | R | The Clinical Information section contains the information provided by the ordering physician: Clinical history, preoperative diagnosis, postoperative diagnosis, clinical laboratory data, specimen(s) description, collection procedure, reason for anatomic pathology procedure.
Contains 1.3.6.1.4.1.19376.1.8.1.2.1 Clinical Information Section (2014‑05‑13 14:38:08) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | where [@typeCode='COMP'] [hl7:section [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.2.1']]] |
| | | cs | 1 … 1 | F | COMP | | bl | 1 … 1 | F | true | | | 0 … 1 | R |
Contains 1.3.6.1.4.1.19376.1.8.1.2.2 Intraoperative Observation Section (2014‑05‑13 19:29:16) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | where [@typeCode='COMP'] [hl7:section [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.2.2']]] |
| | | cs | 1 … 1 | F | COMP | | bl | 1 … 1 | F | true | | | 0 … 1 | R | The Macroscopic Observation section contains the description of the specimen received or obtained by the laboratory (specimen type and state), the gross observation, links to gross images, if taken, processing information and tissue disposition (representative sampling and tissue submitted for additional studies or sent to biorepository.
Contains 1.3.6.1.4.1.19376.1.8.1.2.3 Macroscopic Observation Section (2014‑05‑13 11:57:09) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | where [@typeCode='COMP'] [hl7:section [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.2.3']]] |
| | | cs | 1 … 1 | F | COMP | | bl | 1 … 1 | F | true | | | 0 … 1 | R |
The Microscopic Observation section contains optionally the histopathologic findings of the case and many laboratories use this section to record the results of histochemical and immunohistochemical stains.
Contains 1.3.6.1.4.1.19376.1.8.1.2.4 Microscopic Observation Section (2014‑05‑13 14:25:17) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | where [@typeCode='COMP'] [hl7:section [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.2.4']]] |
| | | cs | 1 … 1 | F | COMP | | bl | 1 … 1 | F | true | | | 0 … 1 | R | The Additional Specific Observation section includes additional pathologic finding(s) and the results of ancillary study(ies) with non-morphological methods (e.g. flow cytometry, cytogenetics, molecular pathology, etc.) and may include diagrams and still images or virtual slides, if taken.
Contains 1.3.6.1.4.1.19376.1.3.10.3.1 Additional Specified Observation Section (2016‑11‑13 14:28:08) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | where [@typeCode='COMP'] [hl7:section [hl7:templateId [@root='1.3.6.1.4.1.19376.1.3.10.3.1']]] |
| | | cs | 1 … 1 | F | COMP | | bl | 1 … 1 | F | true | | | 1 … 1 | M |
The Diagnostic Conclusion section contains diagnoses on all specimens that are delivered to the pathology department from one operation or patient visit to a single clinician on a particular day. The diagnoses for each specimen or group of specimens are reported separately. This section includes additional pathologic finding(s) and the results of ancillary study(ies) and may include diagrams and still images or virtual slides, if taken. In case of cancer, this section includes the cancer checklist.
Contains 1.3.6.1.4.1.19376.1.8.1.2.5 Diagnostic Conclusion Section (2014‑05‑13 19:31:26) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | where [@typeCode='COMP'] [hl7:section [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.2.5']]] |
| | | cs | 1 … 1 | F | COMP | | bl | 1 … 1 | F | true | | | 0 … 1 | R |
The Procedure steps section contains the description of tissue dissection: representative specimens and derived specimens dissected for other ancillary procedures (flow cytometry, cytogenetics, molecular studies, electron microscopy, etc.) or biorepository.
Contains 1.3.6.1.4.1.19376.1.8.1.2.6 Procedure Steps Section (2014‑05‑13 19:33:12) | PaLM Suppl. APSR 2.0‑3: 6.3.1.1 APSR clinical document content module |  |  |  | where [@typeCode='COMP'] [hl7:section [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.2.6']]] |
| | | cs | 1 … 1 | F | COMP | | bl | 1 … 1 | F | true |
|
on Art-Decor
6.2.4 CDA R2 <section> Content Modules
6.2.4.1 Clinical Information <section> - 1.3.6.1.4.1.19376.1.8.1.2.1
6.2.4.1.1 Definition and Purpose
The Clinical Information section contains the information provided by the ordering physician: Clinical history, preoperative diagnosis, postoperative diagnosis, reason for anatomic pathology procedure, clinical laboratory data, specimen collection procedure including target site, performer, specimen type, specimen(s) clinical description, and tumor site in case of a cancer. The only entry for this section is the Problem Organizer Entry module.
6.2.4.1.2 Specification and Example
| Id | 1.3.6.1.4.1.19376.1.8.1.2.1 | Effective Date | valid from 2014‑05‑13 14:38:08 |
|---|
| Status |  Draft Draft | Version Label | 2.0 |
|---|
| Name | ClinicalInformationSection | Display Name | Clinical Information Section |
|---|
| Description | The Clinical Information section contains the information provided by the ordering physician: Clinical history, preoperative diagnosis, postoperative diagnosis, reason for anatomic pathology procedure, clinical laboratory data, information about specimens collected in this case (including target site, performer, specimen type, specimen(s) clinical description, and tumor site in case of a cancer). |
|
| Context | Parent nodes of template element with id 1.3.6.1.4.1.19376.1.8.1.2.1 |
|---|
| Label | PaLM Suppl. 2.0‑3: 6.3.4.1 Clinical information section
|
|---|
| Classification | CDA Section Level Template |
|---|
| Open/Closed | Open (other than defined elements are allowed) |
|---|
| Used by / Uses | | Used by 0 transactions and 1 template, Uses 5 templates | | Used by | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.8.1.1.1 | Containment |  Anatomic Pathology Structured Report Content Module (2.0) Anatomic Pathology Structured Report Content Module (2.0) | 2014‑05‑13 11:57:57 | | Uses | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.8.1.3.6 | Containment |  Problem Organizer (2.0) Problem Organizer (2.0) | 2015‑08‑13 10:24:55 | | 1.3.6.1.4.1.19376.1.8.1.4.2 | Include |  CDA author IHE CDA author IHE | 2016‑06‑21 14:02:11 | | 1.3.6.1.4.1.19376.1.5.3.1.3.1 | Containment |  IHE Reason for Referral Section (2014) IHE Reason for Referral Section (2014) | 2016‑09‑26 07:58:18 | | 1.3.6.1.4.1.19376.1.5.3.1.3.4 | Containment |  IHE History of Present Illness Section (2014) IHE History of Present Illness Section (2014) | 2013‑01‑31 | | 1.3.6.1.4.1.19376.1.5.3.1.3.6 | Containment |  IHE Active Problems Section (2014) IHE Active Problems Section (2014) | 2015‑10‑05 16:02:07 |
|
|
|---|
| Relationship | Specialization: template 2.16.840.1.113883.10.12.201 (2005‑09‑07) |
|---|
| Example | | generated example | <section classCode="DOCSECT" moodCode="EVN">
<templateId root="1.3.6.1.4.1.19376.1.8.1.2.1"/> <code code="22636-5" codeSystem="2.16.840.1.113883.6.1" displayName="Pathology report relevant history"/> <title>CLINICAL INFORMATION SECTION</title> <text/> <languageCode/> <entry xsi:type="ANY" typeCode="COMP" contextConductionInd="true">
<!-- template 1.3.6.1.4.1.19376.1.8.1.3.6 'Problem Organizer' (2015-08-13T10:24:55) -->
</entry> <!-- include template 1.3.6.1.4.1.19376.1.8.1.4.2 'CDA author IHE' (2016-06-21T14:02:11) 0..* C -->
<component>
<!-- template 1.3.6.1.4.1.19376.1.5.3.1.3.1 'IHE Reason for Referral Section' (2016-09-26T07:58:18) -->
</component> <component>
<!-- template 1.3.6.1.4.1.19376.1.5.3.1.3.4 'History of Present Illness Section' (2013-01-31T00:00:00)
-->
</component> <component>
<!-- template 1.3.6.1.4.1.19376.1.5.3.1.3.6 'IHE Active Problems Section' (2015-10-05T16:02:07) -->
</component></section> |
|
|
on Art-Decor
6.2.4.2 Intraoperative Observation <section> - 1.3.6.1.4.1.19376.1.8.1.2.2
6.2.4.2.1 Definition and Purpose
The Intraoperative Observation section contains an intraoperative diagnosis for each specimen examined, the specimen identification and description, intraoperative observation procedure description (frozen section, gross examination, intraoperative cytology) and derived specimen dissected for other ancillary procedures (flow cytometry, cytogenetics, molecular studies, and electron microscopy). The only entry for this section is the Problem Organizer Entry module.
6.2.4.2.2 Specification and Example
 |
LOINC code has been ordered. GH |
on Art-Decor
6.2.4.3 Macroscopic Observation <section> - 1.3.6.1.4.1.19376.1.8.1.2.3
6.2.4.3.1 Definition and Purpose
The Macroscopic Observation section contains the description of the specimen(s) received or obtained by the laboratory (specimen type and state), the gross observation, links to gross images, if taken, processing information and tissue disposition (representative sampling and tissue submitted for additional studies or sent to biorepository. The only entry for this section is the Problem Organizer Entry module.
6.2.4.3.2 Specification and Example
on Art-Decor
6.2.4.4 Microscopic Observation <section> - 1.3.6.1.4.1.19376.1.8.1.2.4
6.2.4.4.1 Definition and Purpose
The Microscopic Observation section contains optionally the histopathologic findings of the case and many laboratories use this section to record the results of histochemical and immunohistochemical stains.The only entry for this section is the Problem Organizer Entry module.
6.2.4.4.2 Specification and Example
on Art-Decor
6.2.4.5 Additionally Specified Observation <section> - 1.3.6.1.4.1.19376.1.3.10.3.1
6.2.4.5.1 Definition and Purpose
The Additionally Specified Observation section includes additional pathologic finding(s) and the results of ancillary study(yes) with non-morphological methods (e.g. flow cytometry, cytogenetics, molecular pathology, etc.) and may include diagrams and still images or virtual slides, if taken. The only entry for this section is the Problem Organizer Entry module.
6.2.4.5.2 Specification and Example
on Art-Decor
6.2.4.6 Diagnostic Conclusion <section> - 1.3.6.1.4.1.19376.1.8.1.2.5
6.2.4.6.1 Definition and Purpose
The Diagnostic Conclusion section contains diagnoses on all specimens that are delivered to the pathology department from one operation or patient visit to a single clinician on a particular day. The diagnoses for each specimen or group of specimens are reported separately. This section includes additional pathologic finding(s) and the results of ancillary study(ies) and may include diagrams and still images or virtual slides, if taken. In case of cancer, this section may also include a the cancer checklist. The only entry for this section is the Problem Organizer Entry module.
6.2.4.6.2 Specification and Example
on Art-Decor
6.2.4.7 Report Textual Summary <section> - 1.3.6.1.4.1.19376.1.8.1.2.7
6.2.4.7.1 Definition and Purpose
The Report Textual Summary section is an optional sub-section of the Diagnostic Conclusion section. This section contains a textual summary of the AP report, which can be extracted from the document and inserted into other clinical documents. It addresses the use case where authors of other medical documents feel the need to include a segment such as "...the pathology report states '[...]'", the text content of this section filling the brackets. This subsection does not contain any entries.
6.2.4.7.2 Specification and Example
Keine Versionen mit Status draft, active, review oder pending.
on Art-Decor
6.2.4.8 Procedure steps <section> - 1.3.6.1.4.1.19376.1.8.1.2.6
6.2.4.8.1 Definition and Purpose
The Procedure steps section contains the description of tissue dissection: representative specimens and derived specimens dissected for other ancillary procedures (flow cytometry, cytogenetics, molecular studies, electron microscopy, etc.) or biorepository. The only entry for this section is the Specimen Procedure Steps Entry module.
6.2.4.8.2 Specification and Example
on Art-Decor
6.2.5 CDA R2 <entry> Content Modules
6.2.5.1 Common Specification for all APSR Entry Content Modules
The unique <entry> Content Module available in all the sections except Procedure Steps <section> of the APSR template is the Problem Organizer <entry>.
The unique <entry> Content Module available in Procedure Steps <section> of the APSR template is Specimen Procedure Step <entry>.
Each <entry> Content Module carries machine-readable data related to one Problem on one specimen or on a group of specimens observed for this section.
Each <entry> Content Module is repeatable below its section, so as to support the use cases where a section reports on more than one specimen or more than one group of specimens.
6.2.5.2 Problem Organizer – 1.3.6.1.4.1.19376.1.8.1.3.6
6.2.5.2.1 Definition and purpose
This Content Module is usable as only <entry> within any Section module except Procedure steps <section>.
The problem organizer groups the battery of observations together with embedded images performed to investigate on a single problem identified on a specimen or group of specimens. If a Problem cannot be addressed specifically the Problem organizer allows also the grouping around one specimen.
6.2.5.2.2 Specification and Example
| Id | 1.3.6.1.4.1.19376.1.8.1.3.6 | Effective Date | valid from 2015‑08‑13 10:24:55 |
|---|
| Status |  Draft Draft | Version Label | 2.0 |
|---|
| Name | ProblemOrganizer | Display Name | Problem Organizer |
|---|
| Description | Template CDA Organizer (prototype, directly derived from POCD_RM000040 MIF)
The problem organizer groups the battery of observations performed to investigate on a single problem identified on a specimen or group of specimens.
|
|
| Context | Parent nodes of template element with id 1.3.6.1.4.1.19376.1.8.1.3.6 |
|---|
| Label | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer
|
|---|
| Classification | CDA Entry Level Template |
|---|
| Open/Closed | Open (other than defined elements are allowed) |
|---|
| Used by / Uses | | Used by 0 transactions and 7 templates, Uses 11 templates | | Used by | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.3.10.3.1 | Containment |  Additional Specified Observation Section (2.0) Additional Specified Observation Section (2.0) | 2016‑11‑13 14:28:08 | | 1.3.6.1.4.1.19376.1.8.1.1.1 |  |  Anatomic Pathology Structured Report Content Module (2.0) Anatomic Pathology Structured Report Content Module (2.0) | 2014‑05‑13 11:57:57 | | 1.3.6.1.4.1.19376.1.8.1.2.1 | Containment |  Clinical Information Section (2.0) Clinical Information Section (2.0) | 2014‑05‑13 14:38:08 | | 1.3.6.1.4.1.19376.1.8.1.2.2 | Containment |  Intraoperative Observation Section (2.0) Intraoperative Observation Section (2.0) | 2014‑05‑13 19:29:16 | | 1.3.6.1.4.1.19376.1.8.1.2.3 | Containment |  Macroscopic Observation Section (2.0) Macroscopic Observation Section (2.0) | 2014‑05‑13 11:57:09 | | 1.3.6.1.4.1.19376.1.8.1.2.4 | Containment |  Microscopic Observation Section (2.0) Microscopic Observation Section (2.0) | 2014‑05‑13 14:25:17 | | 1.3.6.1.4.1.19376.1.8.1.2.5 | Containment |  Diagnostic Conclusion Section (2.0) Diagnostic Conclusion Section (2.0) | 2014‑05‑13 19:31:26 | | Uses | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.8.1.4.2 | Containment |  CDA author IHE CDA author IHE | 2016‑06‑21 14:02:11 | | 1.3.6.1.4.1.19376.1.8.1.4.6 | Containment |  CDA Informant(Header&Body) APSR2 (2.0) CDA Informant(Header&Body) APSR2 (2.0) | 2016‑07‑08 11:22:58 | | 1.3.6.1.4.1.19376.1.8.1.4.7 | Containment |  Additional participant in an entry APSR (Body) Additional participant in an entry APSR (Body) | 2016‑07‑12 18:44:06 | | 1.3.6.1.4.1.19376.1.3.3.1.7 | Containment |  Laboratory Performer (2017) Laboratory Performer (2017) | 2008‑08‑08 | | 1.3.6.1.4.1.19376.1.3.10.9.1 | Include |  X Specimen Identified X Specimen Identified | 2014‑12‑22 15:54:30 | | 1.3.6.1.4.1.19376.1.8.1.4.10 | Containment |  Embedded Image IHE Embedded Image IHE | 2016‑06‑22 16:08:01 | | 2.16.840.1.113883.10.12.307 | Containment |  CDA RegionOfInterest CDA RegionOfInterest | 2005‑09‑07 | | 1.3.6.1.4.1.19376.1.5.3.1.4.2 | Containment |  IHE Comment Entry (2014) IHE Comment Entry (2014) | 2013‑12‑20 | | 1.3.6.1.4.1.19376.1.8.1.4.9 | Containment |  AP Observation Entry (2.0) AP Observation Entry (2.0) | 2014‑05‑14 17:09:54 | | 1.3.6.1.4.1.19376.1.3.1.6 | Containment |  Laboratory Observation (2017) Laboratory Observation (2017) | 2008‑08‑08 | | 2.16.840.1.113883.10.12.324 | Containment |  CDA Reference CDA Reference | 2005‑09‑07 |
|
|
|---|
| Relationship | Specialization: template 2.16.840.1.113883.10.12.305 (2005‑09‑07) |
|---|
| Example | | generated example | <organizer classCode="BATTERY" moodCode="EVN">
<templateId root="1.3.6.1.4.1.19376.1.8.1.3.6"/> <id root="1.2.3.999" extension="--example only--"/> <code code="75326-9" codeSystem="2.16.840.1.113883.6.1" displayName="Problem">
<qualifier>
<name code="116677004" codeSystem="2.16.840.1.113883.6.96" displayName=" Associated topography (attribute)"/> <value nullFlavor="cs" code="all children of "362981000"" codeSystem="2.16.840.1.113883.6.96" displayName="all values from 91723000 (Anatomical structure)"/> </qualifier> </code> <component typeCode="COMP">
<observation>
<code code="75326-9" codeSystem="2.16.840.1.113883.6.1" displayName="Problem">
<value code="115597007" displayName="Description of specimen character (procedure)" codeSystem="2.16.840.1.113883.6.96"/> </code> </observation> </component> <statusCode code="completed"/> <effectiveTime>
<low value="20170131165954"/> </effectiveTime> <author>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.2 'CDA author IHE' (2016-06-21T14:02:11) -->
</author> <informant>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.6 'CDA Informant(Header&Body) APSR2' (2016-07-08T11:22:58) -->
</informant> <participant>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.7 'Additional participant in an entry APSR (Body)' (2016-07-12T18:44:06) -->
</participant> <performer>
<!-- template 1.3.6.1.4.1.19376.1.3.3.1.7 'Laboratory Performer' (2008-08-08T00:00:00) -->
</performer> <!-- include template 1.3.6.1.4.1.19376.1.3.10.9.1 'X Specimen Identified' (2014-12-22T15:54:30) 0..* R -->
<component typeCode="COMP" contextConductionInd="true">
<sequenceNumber value="1"/> <seperatableInd value="false"/> <!-- template 1.3.6.1.4.1.19376.1.8.1.4.10 'Embedded Image IHE' (2016-06-22T16:08:01) -->
</component> <component typeCode="COMP" contextConductionInd="true">
<sequenceNumber value="1"/> <seperatableInd value="false"/> <!-- template 2.16.840.1.113883.10.12.307 'CDA RegionOfInterest' (2005-09-07T00:00:00) -->
</component> <component typeCode="COMP" contextConductionInd="true">
<sequenceNumber value="1"/> <seperatableInd value="false"/> <!-- template 1.3.6.1.4.1.19376.1.5.3.1.4.2 'IHE Comment Entry' (2013-12-20T00:00:00) -->
</component> <component typeCode="COMP" contextConductionInd="true">
<sequenceNumber value="1"/> <seperatableInd value="false"/> <!-- template 1.3.6.1.4.1.19376.1.8.1.4.9 'AP Observation Entry' (2014-05-14T17:09:54) -->
</component> <component typeCode="COMP" contextConductionInd="true">
<sequenceNumber value="1"/> <seperatableInd value="false"/> <!-- template 1.3.6.1.4.1.19376.1.3.1.6 'Laboratory Observation' (2008-08-08T00:00:00) -->
</component> <reference>
<!-- template 2.16.840.1.113883.10.12.324 'CDA Reference' (2005-09-07T00:00:00) -->
</reference></organizer> |
|
| Example | | example for use case #1, problem: invasive breast cancer | <organizer classCode="BATTERY" moodCode="EVN">
<templateId root="1.3.6.1.4.1.19376.1.8.1.3.6"/> <id root="1.3.6.1.4.1.19376.1.8.9.1" extension="A7102400008_Problem1"/> <code code="75326-9" codeSystem="2.16.840.1.113883.6.1" displayName="Problem"/> <statusCode code="completed"/> <effectiveTime>
<low value="201001041605-0500"/> </effectiveTime> <!--The problem is expressed by the result of the observation having the same code as organizer/code-->
<component>
<observation classCode="OBS" moodCode="EVN">
<code code="75326-9" codeSystem="2.16.840.1.113883.6.1" displayName="Problem"/> <value code="C50.9" codeSystem="2.16.840.1.113883.6.3" displayName="Malignant neoplasm of breast, unspecified" codeSystemDisplayName="ICD-10"/> </observation> </component> <component typeCode="COMP" contextConductionInd="true">
<sequenceNumber value="1"/> <seperatableInd value="false"/> <!-- template 1.3.6.1.4.1.19376.1.8.1.4.9 'AP Observation Entry' (2014-05-14T17:09:54) -->
</component> <reference>
<!-- template 2.16.840.1.113883.10.12.324 'CDA Reference' (2005-09-07T00:00:00) -->
</reference></organizer> |
|
| Item | DT | Card | Conf | Description | Label |
|---|
| | 0 … * | R | Problem organizer groups the battery of observations performed to investigate on a single problem identified on a specimen or a group of specimens. | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | @classCode
|
| cs | 1 … 1 | F | BATTERY |  | @moodCode
|
| cs | 1 … 1 | F | EVN |  | hl7:templateId
|
| II | 1 … 1 | M | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  |  | @root
|
| uid | 1 … 1 | F | 1.3.6.1.4.1.19376.1.8.1.3.6 |  | hl7:id
|
| II | 0 … * | R | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | hl7:code
|
| CD (required) | 0 … 1 | R | Problem
| PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  |  | @code
|
| CONF | 0 … 1 | F | 75326-9 |  |  | @codeSystem
|
| 0 … 1 | F | 2.16.840.1.113883.6.1 (Logical Observation Identifier Names and Codes) |  |  | @codeSystemName
|
| 0 … 1 | F | LOINC |  |  | @displayName
|
| 0 … 1 | F | Problem |  | hl7:component
|
| | 0 … 1 | R | Coding of the Problem reported | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP |  |  | hl7:observation
|
| | 0 … 1 | R | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer | | CD (extensible) | 1 … 1 | R | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer | | CONF | 0 … 1 | F | 75326-9 | | 0 … 1 | F | 2.16.840.1.113883.6.1 (Logical Observation Identifier Names and Codes) | | 0 … 1 | F | LOINC | | 0 … 1 | F | Problem | | CR | 0 … * | R | Optional qualifier for separate problems with identical problem type in one specimen, e.g. a urothelial bladder cancer Invasive cancer) and a prostate cancer (invasive cancer) in one cystoprostatectomy specimen. The anatomic structure is able to differentiate.
| PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer | | | Example | Problem in urinary bladder in cystoprostatectomy specimen <qualifier>
<name code="116677004" codeSystem="2.16.840.1.113883.6.96" displayName="Associated topography (attribute)" codeSystemName="SNOMED-CT"/> <value code="302512001" codeSystem="2.16.840.1.113883.6.96" displayName=" Entire urinary bladder (body structure)" codeSystemName="SNOMED-CT"/></qualifier> | | CV | 0 … 1 | R | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer | | cs | 1 … 1 | F | 116677004 | | oid | 1 … 1 | F | 2.16.840.1.113883.6.96 | | st | 1 … 1 | F | Associated topography (attribute) | | CD (extensible) | 0 … * | R | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer | | CONF | 0 … 1 | F | << 91723000 | | 0 … 1 | F | 2.16.840.1.113883.6.96 (SNOMED Clinical Terms) | | 0 … 1 | F | SNOMED-CT | | 0 … 1 | F | all values from Anatomical structure | | CE (extensible) | 0 … 1 | R | Code of the problem reported | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer | | | CONF | | @code shall be "any_code" | | @codeSystem shall be "2.16.840.1.113883.6.3" | | @codeSystemName shall be "any_code" | | @displayName shall be "ICD-10" | | or | | The value of @code should be drawn from value set 1.3.6.1.4.1.19376.1.3.11.7 Problem Type (2016‑07‑11 09:52:19) |
|  | hl7:statusCode
|
| CS (required) | 1 … 1 | M | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer | | | Constraint | The status of the organizer is
completed
if the battery of observations for this problem has been performed. It is
aborted
in case some of the intended observations could not be achieve and have been aborted, and appear as such below the organizer.
| | | CONF | The value of @code shall be drawn from value set 1.3.6.1.4.1.19376.1.3.11.2 (DYNAMIC) | Error: Cannot find value set "1.3.6.1.4.1.19376.1.3.11.2" |
|
|  | hl7:effectiveTime
|
| IVL_TS | 1 … 1 | M | Organizer time.
The period of time (possibly reduced to a point in time) during which the information was collected and assembled.
| PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | hl7:author
|
| | 0 … * | C | Author
Source: PaLM Suppl. APSR 2.0-3: 6.3.6.2
Contains 1.3.6.1.4.1.19376.1.8.1.4.2 CDA author IHE (2016‑06‑21 14:02:11) | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | where [hl7:author [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.2']]] |
| | | | Constraint | The author SHALL be present if it is different from the main author of the report. For instance the author could be the ordering physician contributing to the Clinical Information section, inside a report authored by the pathologist.
|  | hl7:informant
|
| | 0 … * | R | Informant
The informant is an actor (person and organization) who provided some of the clinical information carried by this organizer.
Source: PaLM Suppl. APSR 2.0-3:
6.3.6.5
Contains 1.3.6.1.4.1.19376.1.8.1.4.6 CDA Informant(Header&Body) APSR2 (2016‑07‑08 11:22:58) | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | where [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.6']] |
| |  | hl7:participant
|
| | 0 … * | R | Transcriptionist, Device, Responsible, Validator
Source: PaLM Suppl. APSR 2.0-3:
6.3.6.6
Contains 1.3.6.1.4.1.19376.1.8.1.4.7 Additional participant in an entry APSR (Body) (2016‑07‑12 18:44:06) | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | where [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.7']] |
| | | | Constraint | participationType "ENT", "DEV", "RESP", "AUTHEN"
|  | hl7:performer
|
| | 0 … 1 | C | Performing lab.
The performing laboratory is present at this level only if this particular problem on this particular specimen was investigated by a (subcontractor) distinct laboratory from the one issuing the consolidated report
Source:
PaLM TF-3: 6.3.2.20
Contains 1.3.6.1.4.1.19376.1.3.3.1.7 Laboratory Performer (2008‑08‑08) | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | where [hl7:templateId [@root='1.3.6.1.4.1.19376.1.3.3.1.7']] |
| | | Included | 0 … * | R | from 1.3.6.1.4.1.19376.1.3.10.9.1 X Specimen Identified (2014‑12‑22 15:54:30)
Specimen identification outside an AP observation for differentiating or restituting the problem type
Source: PaLM Suppl. APSR 2.0-3: 6.3.6.9
|  | hl7:specimen
|
| | 0 … * | R | Required in XD-LAB when more than one specimen is documented at this level. Always required in APSR.
| PaLM Suppl. APSR 2.0‑3: 6.3.6.9 X Specimen identified |  |  | @typeCode
|
| cs | 0 … 1 | F | SPC |  |  | hl7:specimenRole
|
| | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.6.9 X Specimen identified | | cs | 0 … 1 | F | SPEC | | II | 1 … 1 | R | Specimen ID, coming from the LIS | PaLM Suppl. APSR 2.0‑3: 6.3.6.9 X Specimen identified |  | hl7:component
|
| | 0 … * | R | Embedded image
This organizer may carry an image focusing on the problem, either directly embedded or encapsulated within a region of interest.
Contains 1.3.6.1.4.1.19376.1.8.1.4.10 Embedded Image IHE (2016‑06‑22 16:08:01) | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | where [hl7:observationMedia [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.10']]] |
| |  |  | @typeCode
|
| cs | 0 … 1 | F | COMP |  |  | @contextConductionInd
|
| bl | 0 … 1 | F | true | | | Constraint | [@classCode="ROIOVL" and moodCode="EVN"] |  |  | hl7:sequenceNumber
|
| INT | 0 … 1 | | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  |  | hl7:seperatableInd
|
| BL | 0 … 1 | | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | hl7:component
|
| | 0 … * | R | Region of interest
This organizer may carry an image focusing on the problem, either directly embedded or encapsulated within a region of interest.
In the latter case by an entryRelationship @typeCode="SUBJ"
Contains 2.16.840.1.113883.10.12.307 CDA RegionOfInterest (2005‑09‑07) | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | where [@typeCode='COMP'] [hl7:regionOfInterest [hl7:templateId [@root='2.16.840.1.113883.10.12.307']]] |
| |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP |  |  | @contextConductionInd
|
| bl | 0 … 1 | F | true | | | Constraint | [@classCode="ROIOVL" and moodCode="EVN"] |  |  | hl7:sequenceNumber
|
| INT | 0 … 1 | | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  |  | hl7:seperatableInd
|
| BL | 0 … 1 | | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | hl7:component
|
| | 0 … * | R | General comment on this particular problem
Source: PCC TF-2: 6.3.4.6
Contains 1.3.6.1.4.1.19376.1.5.3.1.4.2 IHE Comment Entry (2013‑12‑20) | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | where [@typeCode='COMP'] [hl7:act [hl7:templateId [@root='2.16.840.1.113883.10.20.1.40'] and hl7:templateId [@root='1.3.6.1.4.1.19376.1.5.3.1.4.2']]] |
| |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP |  |  | @contextConductionInd
|
| bl | 0 … 1 | F | true |  |  | hl7:sequenceNumber
|
| INT | 0 … 1 | | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  |  | hl7:seperatableInd
|
| BL | 0 … 1 | | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | hl7:component
|
| | 0 … * | R | Any kind of AP observation, for complex observations, e.g. for TNM, ICD-O-3, or Assessment scales, the appropriate templates may be used.
Source: PaLM Suppl. APSR 2.0-3: 6.3.6.7
Contains 1.3.6.1.4.1.19376.1.8.1.4.9 AP Observation Entry (2014‑05‑14 17:09:54) | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | where [@typeCode='COMP'] [hl7:observation [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.9']]] |
| |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP |  |  | @contextConductionInd
|
| bl | 0 … 1 | F | true |  |  | hl7:sequenceNumber
|
| INT | 0 … 1 | | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  |  | hl7:seperatableInd
|
| BL | 0 … 1 | | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | hl7:component
|
| | 0 … * | C | Laboratory observation
Contains 1.3.6.1.4.1.19376.1.3.1.6 Laboratory Observation (2008‑08‑08) | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | where [@typeCode='COMP'] [hl7:observation [hl7:templateId [@root='1.3.6.1.4.1.19376.1.3.1.6']]] |
| |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP |  |  | @contextConductionInd
|
| bl | 0 … 1 | F | true |  |  | hl7:sequenceNumber
|
| INT | 0 … 1 | | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  |  | hl7:seperatableInd
|
| BL | 0 … 1 | | | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |  | hl7:reference
|
| | 0 … * | R | Reference to an external document, or to external organizers, or to external observations, e.g. concerning molecular pathology or genetic testing report
Contains 2.16.840.1.113883.10.12.324 CDA Reference (2005‑09‑07) | PaLM Suppl. 2.0‑3: 6.3.5.2 Problem organizer |
|
on Art-Decor
6.2.5.3 Specimen Procedure Step <entry> - 1.3.6.1.4.1.19376.1.3.10.4.1
6.2.5.3.1 Definition and purpose
The Specimen Procedure Step <entry> Content Modul contains in machine-readable form all the information concerning one specimen or a group of specimens together with its container(s). It is usable within a Procedure Steps <section> Content Module only.
This Content Module structures the machine-readable data, which characterize the specimens and the procedures of their collection and processing (identifiers and types, time intervals, performers, approach site, target site). By referencing the child procedure ID via an entryRelationship the entry is used in an iterative manner for each single step of specimen collection and processing, which results in derived (child) specimen in and on the appropriate containers. The resulting specimen is the participant in the procedure according the CDA-RIM (fig. 6.2.6.11.1-1). Specimen and their container carry IDs as well as further attributes, which are defined in the HL7 Specimen DAM.
HL7 DAM Specimen Release 1.
According to the CDA RIM in the Content Module further supporting Content Modules for Participant, and Playing Entity are needed, which have the (preliminary) OIDs 1.3.6.1.4.1.19376.1.3.10.9.20, 1.3.6.1.4.1.19376.1.3.10.9.21)
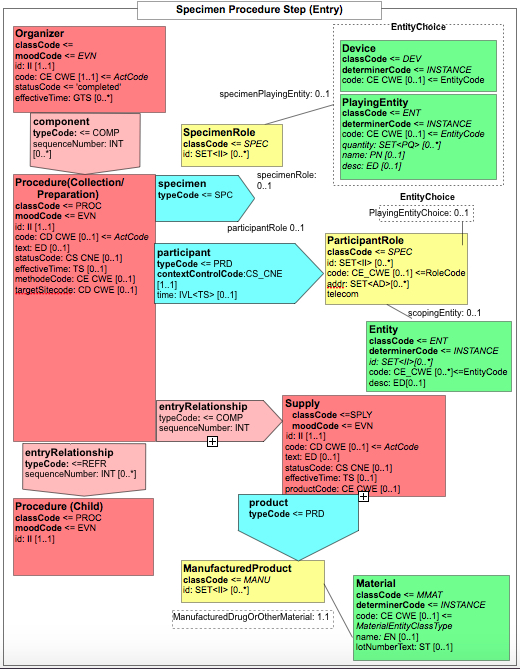
Figure 6.2.5.3.2-1 CDA-RMIM of the Specimen Procedure Steps <entry>
The Code systems and Value sets MAY be organized organ-specific and represented e.g. by PathLex.
6.2.5.3.2 Specification and Example
| Id | 1.3.6.1.4.1.19376.1.3.10.4.1 | Effective Date | valid from 2016‑07‑08 13:20:59There are versions of templates with this id:- SpecimenProcedureStep as of 2016‑07‑08 13:20:59
- SpecimenProcedureStep as of 2014‑07‑29 16:02:02
|
|---|
| Status |  Draft Draft | Version Label | 2.0 |
|---|
| Name | SpecimenProcedureStep | Display Name | Specimen Procedure Step |
|---|
| Description | Template CDA Procedure (prototype, directly derived from POCD_RM000040 MIF)
for Specimen procedure step in APSR2.
This entry collects all the information of source, method and result of a specimen procedure from the collection out of the patient through the final product of a stained histologic section or cytologic smear on a glass slide, or a WSI of such a slide. It reflects the workflow and the probe tracking of a pathology laboratory.
|
|
| Context | Parent nodes of template element with id 1.3.6.1.4.1.19376.1.3.10.4.1 |
|---|
| Label | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps
|
|---|
| Classification | CDA Entry Level Template |
|---|
| Open/Closed | Open (other than defined elements are allowed) |
|---|
| Used by / Uses | | Used by 0 transactions and 4 templates, Uses 8 templates | | Used by | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.3.10.4.1 | Containment |  Specimen Procedure Step (2.0) Specimen Procedure Step (2.0) | 2016‑07‑08 13:20:59 | |  Circular reference found with 1.3.6.1.4.1.19376.1.3.10.4.1, please check Circular reference found with 1.3.6.1.4.1.19376.1.3.10.4.1, please check | | 1.3.6.1.4.1.19376.1.3.10.4.1 |  |  Specimen Procedure Step (1.0) Specimen Procedure Step (1.0) | 2014‑07‑29 16:02:02 | |  Circular reference found with 1.3.6.1.4.1.19376.1.3.10.4.1, please check Circular reference found with 1.3.6.1.4.1.19376.1.3.10.4.1, please check | | 1.3.6.1.4.1.19376.1.8.1.2.6 |  |  Procedure Steps Section (2.0) Procedure Steps Section (2.0) | 2014‑05‑13 19:33:12 | | 1.3.6.1.4.1.19376.1.8.1.1.1 |  |  Anatomic Pathology Structured Report Content Module (2.0) Anatomic Pathology Structured Report Content Module (2.0) | 2014‑05‑13 11:57:57 | | Uses | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.3.10.9.1 | Include |  X Specimen Identified X Specimen Identified | 2014‑12‑22 15:54:30 | | 1.3.6.1.4.1.19376.1.3.3.1.7 | Containment |  Laboratory Performer (2017) Laboratory Performer (2017) | 2008‑08‑08 | | 1.3.6.1.4.1.19376.1.8.1.4.2 | Containment |  CDA author IHE CDA author IHE | 2016‑06‑21 14:02:11 | | 1.3.6.1.4.1.19376.1.3.10.9.44 | Containment |  CDA Participant (Body) Procedure Steps APSR2 (2.0) CDA Participant (Body) Procedure Steps APSR2 (2.0) | 2014‑10‑26 17:06:28 | | 1.3.6.1.4.1.19376.1.3.10.9.22 | Containment |  CDA Supply Container APSR2 (2.0) CDA Supply Container APSR2 (2.0) | 2016‑07‑29 12:09:33 | | 1.3.6.1.4.1.19376.1.3.1.3 | Containment |  Specimen Received (2017) Specimen Received (2017) | 2008‑08‑08 | | 1.3.6.1.4.1.19376.1.3.10.4.1 | Containment |  Specimen Procedure Step (2.0) Specimen Procedure Step (2.0) | 2016‑07‑08 13:20:59 | | 2.16.840.1.113883.10.12.324 | Containment |  CDA Reference CDA Reference | 2005‑09‑07 |
|
|
|---|
| Relationship | Adaptation: template 2.16.840.1.113883.10.12.306 (2005‑09‑07) |
|---|
| Example | | generated example | <procedure negationInd="false" classCode="PROC" moodCode="EVN">
<templateId root="1.3.6.1.4.1.19376.1.3.10.4.1"/> <id root="1.2.3.999" extension="--example only--"/> <code code="117617002" displayName="Immunohistochemistry procedure (procedure)" codeSystem="2.16.840.1.113883.5.96">
<qualifier>
<name code="246094008 or 246355002" codeSystem="2.16.840.1.113883.6.96" displayName="Component investigated (attribute) or Supporting structure (attribute)"/> <value code="23307004" codeSystem="2.16.840.1.113883.6.96" displayName="Estrogen receptor (substance)"/> </qualifier> </code> <text/> <statusCode code="completed"/> <effectiveTime>
<low value="20161110104817"/> </effectiveTime> <targetSiteCode code="441652008" codeSystem="2.16.840.1.113883.6.96" displayName="Formalin-fixed paraffin-embedded tissue specimen (specimen)"/> <specimen typeCode="SPC">
<specimenRole classCode="SPEC">
<id/> </specimenRole> </specimen> <performer>
<!-- template 1.3.6.1.4.1.19376.1.3.3.1.7 'Laboratory Performer' (2008-08-08T00:00:00) -->
</performer> <author>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.2 'CDA author IHE' (2016-06-21T14:02:11) -->
</author> <participant>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.44 'CDA Participant (Body) Procedure Steps APSR2' (2014-10-26T17:06:28) -->
</participant> <entryRelationship negationInd="false" typeCode="COMP" inversionInd="false" contextConductionInd="true">
<seperatableInd value="false"/> <sequenceNumber value="1"/> <!-- template 1.3.6.1.4.1.19376.1.3.10.9.22 'CDA Supply Container APSR2' (2016-07-29T12:09:33) -->
</entryRelationship> <entryRelationship negationInd="false" typeCode="COMP" inversionInd="false" contextConductionInd="true">
<seperatableInd value="false"/> <!-- template 1.3.6.1.4.1.19376.1.3.1.3 'Specimen Received' (2008-08-08T00:00:00) -->
</entryRelationship> <entryRelationship negationInd="false" typeCode="REFR" inversionInd="false" contextConductionInd="true">
<seperatableInd value="false"/> <!-- template 1.3.6.1.4.1.19376.1.3.10.4.1 'Specimen Procedure Step' (2016-07-08T13:20:59) -->
</entryRelationship> <reference>
<!-- template 2.16.840.1.113883.10.12.324 'CDA Reference' (2005-09-07T00:00:00) -->
</reference></procedure> |
|
| Item | DT | Card | Conf | Description | Label |
|---|
| | 0 … * | R | | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  | @classCode
|
| cs | 1 … 1 | F | PROC |  | @moodCode
|
| cs | 1 … 1 | F | EVN |  | hl7:templateId
|
| II | 1 … 1 | R | | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  |  | @root
|
| uid | 1 … 1 | F | 1.3.6.1.4.1.19376.1.3.10.4.1 |  | hl7:id
|
| II | 0 … * | R | Procedure ID, coming from the LIS.
May be the target (referenced) ID for the child procedure. | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  | hl7:code
|
| CD (extensible) | 1 … 1 | M | Coded procedure | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps | | | Constraint | for specimen collection procedure codes for targetSite or SNOMED CT have to be used, for specimen processing (down step the procedures) SNOMED CT is preferred, DICOM could be used if available
| | | CONF | | The value of @code should be drawn from value set 1.3.6.1.4.1.19376.1.3.11.10 Specimen Collection and Processing (2016‑05‑31 15:09:59) |
| | | Example | for use case #1, specimen collection <code code="122548005" codeSystem="2.16.840.1.113883.6.96" displayName="Biopsy of breast (procedure)" codeSystemName="SNOMED-CT"/> | | | Example | for use case #1, grossing & embedding <code code="40923002" codeSystem="2.16.840.1.113883.6.96" displayName="Tissue processing technique, routine, embed, cut and stain, per surgical specimen (procedure)"/> | | | Example | for use case #1, sectioning & immunostaining <code code="117617002" codeSystem="2.16.840.1.113883.6.96" displayName="Immunohistochemistry procedure (procedure)"/> |  |  | hl7:qualifier
|
| CR (extensible) | 0 … * | C | Qualifier for staining or other procedures which don´t have values in the vocabulary used.
| PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps | | | Constraint | Used only in staining and other procedures without values in SCT or LOINC or DICOM vocabulary, e.g. immune stains
| | | Example | for use case #1, grossing & embedding <qualifier>
<name code="246355002" displayName="Supporting structure (attribute)" codeSystem="2.16.840.1.113883.6.96"/> <value code="702941008" displayName="Paraffin embedding (qualifier value)" codeSystem="2.16.840.1.113883.6.96" codeSystemName="SNOMED-CT"/></qualifier> | | | Example | for use case #1, Estrogen receptor staining <qualifier>
<name code="246094008" displayName="Component investigated (attribute)" codeSystem="2.16.840.1.113883.6.96"/> <value code="23307004" displayName="Estrogen receptor (substance)" codeSystem="2.16.840.1.113883.6.96"/></qualifier> | | | Example | for use case #1, ISH Her-2-neu staining <qualifier>
<name code="246094008" displayName="Component investigated (attribute)" codeSystem="2.16.840.1.113883.6.96"/> <value code="164870" displayName="ONCOGENE ERBB2" codeSystem="2.16.840.1.113883.6.174" codeSystemName="OMIM"/></qualifier> | | CV (extensible) | 1 … 1 | R | | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps | | cs | 0 … 1 | F | 246094008_or_246355002 | | oid | 0 … 1 | F | 2.16.840.1.113883.6.96 | | st | 0 … 1 | F | Component investigated (attribute) or Supporting structure (attribute) | | CD (extensible) | 1 … 1 | R | | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps | | cs | 1 … 1 | R | | | | CONF | | @code shall be "<<105590001 | Substance (substance) |" | | @codeSystem shall be "2.16.840.1.113883.6.96" | | @codeSystemName shall be "SNOMED-CT" | | @displayName shall be "values from substance axis, e.g. Estrogen receptor" | | or | | @code shall be "values from G axis" | | @codeSystem shall be "2.16.840.1.113883.6.174" | | @codeSystemName shall be "OMIM" | | @displayName shall be "values from G axis, e.g. erb-b2" | | or | | @code shall be "<<272394005 | Technique (qualifier value) |" | | @codeSystem shall be "2.16.840.1.113883.6.96" | | @codeSystemName shall be "SNOMED-CT" | | @displayName shall be "values from technique axis, e.g. Paraffin embedded (qualifier)" |
|  | hl7:text
|
| ED | 0 … 1 | R | | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps | | | Example | specimen collection procedure <text>ULTRASOUND GUIDED NEEDLE CORE BIOPSY</text> | | | Example | specimen processing procedure <text>CUTTING A SLIDE FROM A PARAFFIN BLOCK</text> |  | hl7:statusCode
|
| CS (required) | 0 … 1 | R | | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps | | | CONF | | The value of @code shall be drawn from value set 2.16.840.1.113883.1.11.15933 ActStatus (DYNAMIC) |
|  | hl7:effectiveTime
|
| IVL_TS | 0 … 1 | R | | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  | hl7:approachSiteCode
|
| CD (extensible) | 0 … 1 | R | Approach site in specimen collection | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  |  | @code
|
| CONF | 0 … 1 | F | any_code |  |  | @codeSystem
|
| 0 … 1 | F | 2.16.840.1.113883.5.1052 (Act Site) |  |  | @codeSystemName
|
| 0 … 1 | F | any_code |  |  | @displayName
|
| 0 … 1 | F | ActSite |  | hl7:targetSiteCode
|
| CD (extensible) | 0 … 1 | R | Target site in body or relative parent relationship in case of specimen processing | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps | | | CONF | | @code shall be "<<123037004 | Body structure (body structure) |" | | @codeSystem shall be "2.16.840.1.113883.6.96" | | @codeSystemName shall be "SCT" | | @displayName shall be "all children of Body structure (body structure)" | | or | | @code shall be "any_code" | | @codeSystem shall be "2.16.840.1.113883.5.1052" | | @codeSystemName shall be "ActSite" | | @displayName shall be "any_code" | | or | | The value of @code should be drawn from value set 1.3.6.1.4.1.19376.1.3.11.9 Procedure Site (2016‑06‑01 18:46:15) |
| | | Example | for use case #1, specimen collection <targetSiteCode code="110497008" displayName="Lower outer quadrant of right breast (body structure)" codeSystem="2.16.840.1.113883.6.96"/> | | | Example | for use case #1, grossing & embedding <targetSiteCode code="309050000" displayName="Body substance sample" codeSystem="2.16.840.1.113883.6.96"/> |  |  | hl7:qualifier
|
| CR (extensible) | 0 … * | C | optional qualifiers for specifying body structures or / and laterality | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps | | | Example | for use case #1, (optional) specification of body structure for specimen collection <qualifier>
<name code="118169006" codeSystem="2.16.840.1.113883.6.96" displayName="Specimen source topography (attribute)" codeSystemName="SNOMED-CT"/> <value code="255495000" codeSystem="2.16.840.1.113883.6.96" displayName="Right lower quadrant (qualifier value)" codeSystemName="SNOMED-CT"/></qualifier> | | CV (extensible) | 1 … 1 | R | | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps | | st | 0 … 1 | F | Specimen source topography | | oid | 1 … 1 | F | 2.16.840.1.113883.6.96 | | cs | 1 … 1 | F | 118169006 | | CD (extensible) | 0 … * | R | | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps | | CONF | 0 … 1 | | @code shall be out of choice:- <<272099008
- Descriptor (qualifier value)
| | 0 … 1 | F | 2.16.840.1.113883.6.96 (SNOMED Clinical Terms) | | 0 … 1 | F | SCT | | 0 … 1 | F | all children of "Descriptor, qualifier values", e.g. right lower quadrantt |  | hl7:methodCode
|
| CD (extensible) | 0 … * | R | Identifies the technique used to perform a procedure
| PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  |  | @codeSystem
|
| cs | 1 … 1 | F | 2.16.840.1.113883.5.1065 | | Included | 0 … 1 | R | from 1.3.6.1.4.1.19376.1.3.10.9.1 X Specimen Identified (2014‑12‑22 15:54:30)
Parent specimen with parent ID | | | Example | for use case #1, parent specimen ID in grossing & embedding <specimen typeCode="SPC">
<specimenRole classCode="SPEC">
<!-- Parent specimen ID -->
<id root="1.3.6.1.4.1.19376.1.8.9.1" extension="A7102400008"/> </specimenRole></specimen> |  | hl7:specimen
|
| | 0 … 1 | R | Required in XD-LAB when more than one specimen is documented at this level. Always required in APSR.
| PaLM Suppl. APSR 2.0‑3: 6.3.6.9 X Specimen identified |  |  | @typeCode
|
| cs | 0 … 1 | F | SPC |  |  | hl7:specimenRole
|
| | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.6.9 X Specimen identified | | cs | 0 … 1 | F | SPEC | | II | 1 … 1 | R | Specimen ID, coming from the LIS | PaLM Suppl. APSR 2.0‑3: 6.3.6.9 X Specimen identified |  | hl7:performer
|
| | 0 … 1 | R | Contains 1.3.6.1.4.1.19376.1.3.3.1.7 Laboratory Performer (2008‑08‑08) | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  | where [hl7:templateId [@root='1.3.6.1.4.1.19376.1.3.3.1.7']] |
| |  | hl7:author
|
| | 0 … * | C | Contains 1.3.6.1.4.1.19376.1.8.1.4.2 CDA author IHE (2016‑06‑21 14:02:11) | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  | where [hl7:author [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.2']]] |
| |  | hl7:participant
|
| | 1 … * | M | One or more specimen (with additives), which participates as product of the procedure
Contains 1.3.6.1.4.1.19376.1.3.10.9.44 CDA Participant (Body) Procedure Steps APSR2 (2014‑10‑26 17:06:28) | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  | where [not(@nullFlavor)] |
| |  | hl7:entryRelationship
|
| | 0 … * | R | Artificial material (manufactured product) which
containes
the specimen
Contains 1.3.6.1.4.1.19376.1.3.10.9.22 CDA Supply Container APSR2 (2016‑07‑29 12:09:33) | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  | where [@typeCode='COMP'] [hl7:supply [hl7:templateId [@root='1.3.6.1.4.1.19376.1.3.10.9.22']]] |
| |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP |  |  | @contextConductionInd
|
| bl | 0 … 1 | F | true | | | Constraint | for manufactured product
classCode = MANU
for DrugOrOtherMaterial
classCode = MMAT
code from MaterialEntityClassType
|  | hl7:entryRelationship
|
| | 0 … 1 | R | Specimen arrival in Lab
Contains 1.3.6.1.4.1.19376.1.3.1.3 Specimen Received (2008‑08‑08) | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  | where [@typeCode='COMP'] [hl7:act [hl7:templateId [@root='1.3.6.1.4.1.19376.1.3.1.3']]] |
| |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP |  |  | @contextConductionInd
|
| bl | 0 … 1 | F | true |  | hl7:entryRelationship
|
| | 0 … * | R | Referencing mechanism to the ID of the child procedures, giving a lis of child procedure IDs
Contains 1.3.6.1.4.1.19376.1.3.10.4.1 Specimen Procedure Step (2016‑07‑08 13:20:59) | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |  | where [@typeCode='REFR'] [hl7:procedure [hl7:templateId [@root='1.3.6.1.4.1.19376.1.3.10.4.1']]] |
| |  |  | @typeCode
|
| cs | 1 … 1 | F | REFR |  |  | @contextConductionInd
|
| bl | 0 … 1 | F | true | | | Constraint | contains only ID of the child procedure, which is fully described in a dedicated entry further down in the Procedure step section. |  | hl7:reference
|
| | 0 … * | R | Reference to an external document, or to external procedures, e.g. concerning molecular pathology or genetic testing report
Contains 2.16.840.1.113883.10.12.324 CDA Reference (2005‑09‑07) | PaLM Suppl. 2.0‑3: 6.3.5.3 Specimen procedure steps |
|
on Art-Decor
6.2.6 CDA R2 Child Element Content Modules
This section specifies the Content Modules designed for child elements. A child element is a child of the CDA header or a child of a <section>, or an element nested at various depths below an <entry>, or an element appearing at some combination of these locations.
6.2.6.1.1 Definition and purpose
This Content Module is usable only in the CDA header.
This Content Module is used only in the situation where the specimen was not collected by the ordering physician. (See use cases in volume 1)
6.2.6.1.2 Specification and Example
| Id | 1.3.6.1.4.1.19376.1.8.1.4.1 | Effective Date | valid from 2016‑06‑13 14:21:13 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | CDAParticipantSpecimenCollector | Display Name | CDA Participant Specimen Collector |
|---|
| Description | Template CDA participant (prototype, directly derived from POCD_RM000040 MIF)
This Content Module is usable only in the CDA header.
This Content Module is used only in the situation where the specimen was not collected by the ordering physician.
|
|
| Label | PaLM Suppl. APSR 2.0‑3:6.3.6.1 Specimen collector
|
|---|
| Classification | CDA Header Level Template |
|---|
| Open/Closed | Open (other than defined elements are allowed) |
|---|
| Used by / Uses | | Used by 0 transactions and 1 template, Uses 2 templates | | Used by | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.8.1.1.1 | Include |  Anatomic Pathology Structured Report Content Module (2.0) Anatomic Pathology Structured Report Content Module (2.0) | 2014‑05‑13 11:57:57 | | Uses | as | Name | Version |
|---|
| 2.16.840.1.113883.10.12.152 | Containment |  CDA Person CDA Person | 2005‑09‑07 | | 2.16.840.1.113883.10.12.151 | Containment |  CDA Organization CDA Organization | 2005‑09‑07 |
|
|
|---|
| Relationship | Specialization: template 2.16.840.1.113883.10.12.108 (2005‑09‑07) |
|---|
| Example | | generated example | <participant typeCode="DIST" contextControlCode="OP">
<templateID root="1.3.6.1.4.1.19376.1.8.1.4.1"/> <time>
<low value="20170127121035"/> </time> <associatedEntity classCode="PROV">
<id root="1.2.3.999" extension="--example only--"/> <code code="--code--" codeSystem="2.16.840.1.113883.5.111"/> <addr>addr</addr> <telecom/> <associatedPerson>
<!-- template 2.16.840.1.113883.10.12.152 'CDA Person' (dynamic) -->
</associatedPerson> <scopingOrganization>
<!-- template 2.16.840.1.113883.10.12.151 'CDA Organization' (dynamic) -->
</scopingOrganization> </associatedEntity></participant> |
|
|
on Art-Decor
6.2.6.2 Author – 1.3.6.1.4.1.19376.1.8.1.4.2
6.2.6.2.1 Definition and purpose
This Content Module is usable in the CDA header, in a <section> and at various depths of an <entry>.
It describes an author having contributed to the document wholly or to a portion of it (e.g., a section, an observation, a group of observations).
A given document or any delimited portion of it may have more than one author.
An author MAY be a person or a device (manufactured device or software system). In both cases the scoping organization MAY be described.
6.2.6.2.2 Specification and Example
on Art-Decor
6.2.6.3 Content Validator – 1.3.6.1.4.1.19376.1.8.1.4.3
6.2.6.3.1 Definition and purpose
This Content Module is usable only in the CDA header.
It describes a pathologist having verified the content of the report, using the element authenticator. This element authenticator is used when the pathologist having verified the content of the report is distinct from the pathologist assuming the legal responsibility for this report, described in the legalAuthenticator element.
The report MAY have zero or more Content Validators.
6.2.6.3.2 Specification and Example
on Art-Decor
6.2.6.4 Container in Specimen Procedure Step - 1.3.6.1.4.1.19376.1.3.10.9.22
6.2.6.4.1 Definition and purpose
This Supporting Content Module is usable in the Specimen Procedure Steps <entry> (see 6.2.6.4). It describes the properties of containers, in or on which the specimens are processed. The relations between container and specimen are described in the HL7 Specimen DAM.
HL7 DAM Specimen Release 1.
For Anatomic Pathology the CDA Content Modules "Material" and "ManufacturedMaterial" were modified under the (preliminary) OIDs 1.3.6.1.4.1.19376.1.3.10.9.23 and 1.3.6.1.4.1.19376.1.3.10.9.24
6.2.6.4.2 Specification and Example
on Art-Decor
6.2.6.5 Informant – 1.3.6.1.4.1.19376.1.8.1.4.6
6.2.6.5.1 Definition and purpose
This Content Module is usable in the CDA header, in a <section> and within an <entry>.
It describes a person having provided some piece of relevant information for the document.
A <ClinicalDocument> or a <section> or any kind of act below an <entry>, MAY have zero or more informant.
6.2.6.5.2 Specification and Example
on Art-Decor
6.2.6.6 Additional participant in an entry - 1.3.6.1.4.1.19376.1.8.1.4.7
6.2.6.6.1 Definition and purpose
This Content Module is usable only within an <entry> element.
Additional participants MAY take part in any organizer as well as in any observation of an APSR. These participants MAY be any of these 4:
- Validator: This is the same participation as Content Validator in the header of the report: a pathologist having verified the content (of this particular subset of results).
- Device: A device used to produce this particular subset of results.
- Responsible: The director of a laboratory (described in a performer element at the same level) who produced this particular subset of results.
- Transcriptionist: This is the same participation as dataEnterer in the header of the report: a staff who entered, possibly from dictation, this particular subset of results.
6.2.6.6.2 Specification and Example
| Id | 1.3.6.1.4.1.19376.1.8.1.4.7 | Effective Date | valid from 2016‑07‑12 18:44:06 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | AdditionalParticipantAPSR | Display Name | Additional participant in an entry APSR (Body) |
|---|
| Description | Template CDA Participant (Body) (prototype, directly derived from POCD_RM000040 MIF) |
|---|
| Label | PaLM Suppl. APSR 2.0‑3: 6.3.6.6 Additional participant
|
|---|
| Classification | CDA Entry Level Template |
|---|
| Open/Closed | Open (other than defined elements are allowed) |
|---|
| Used by / Uses | | Used by 0 transactions and 18 templates, Uses 2 templates | | Used by | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.3.10.4.2 | Containment |  TNM Stage Observation (2.0) TNM Stage Observation (2.0) | 2014‑05‑13 15:45:13 | | 1.3.6.1.4.1.19376.1.3.10.4.1 |  |  Specimen Procedure Step (1.0) Specimen Procedure Step (1.0) | 2014‑07‑29 16:02:02 | | 1.3.6.1.4.1.19376.1.3.10.4.3 | Containment |  ICD-O-3 Typing and Grading Observation (2.0) ICD-O-3 Typing and Grading Observation (2.0) | 2015‑11‑29 17:03:18 | | 1.3.6.1.4.1.19376.1.3.10.4.4 | Containment |  Assessment Scales Observation for Scoring Systems APSR2 (2.0) Assessment Scales Observation for Scoring Systems APSR2 (2.0) | 2016‑10‑06 13:12:00 | | 1.3.6.1.4.1.19376.1.3.10.9.26 | Containment |  TNM N-Observation (2.0) TNM N-Observation (2.0) | 2014‑12‑02 16:34:50 | | 1.3.6.1.4.1.19376.1.3.10.9.27 | Containment |  TNM M-Observation (2.0) TNM M-Observation (2.0) | 2014‑12‑02 16:32:30 | | 1.3.6.1.4.1.19376.1.3.10.9.37 | Containment |  TNM Number of nodes (2.0) TNM Number of nodes (2.0) | 2014‑12‑02 16:48:36 | | 1.3.6.1.4.1.19376.1.3.10.9.43 | Containment |  Assessment Scoring Item APSR 2.0 (2.0) Assessment Scoring Item APSR 2.0 (2.0) | 2016‑10‑11 10:26:17 | | 1.3.6.1.4.1.19376.1.3.10.9.42 |  |  Assessment Scoring System APSR 2.0 (2.0) Assessment Scoring System APSR 2.0 (2.0) | 2016‑10‑10 11:33:36 | | 1.3.6.1.4.1.19376.1.8.1.3.6 | Containment |  Problem Organizer (2.0) Problem Organizer (2.0) | 2015‑08‑13 10:24:55 | | 1.3.6.1.4.1.19376.1.3.10.3.1 |  |  Additional Specified Observation Section (2.0) Additional Specified Observation Section (2.0) | 2016‑11‑13 14:28:08 | | 1.3.6.1.4.1.19376.1.8.1.1.1 |  |  Anatomic Pathology Structured Report Content Module (2.0) Anatomic Pathology Structured Report Content Module (2.0) | 2014‑05‑13 11:57:57 | | 1.3.6.1.4.1.19376.1.8.1.2.1 |  |  Clinical Information Section (2.0) Clinical Information Section (2.0) | 2014‑05‑13 14:38:08 | | 1.3.6.1.4.1.19376.1.8.1.2.2 |  |  Intraoperative Observation Section (2.0) Intraoperative Observation Section (2.0) | 2014‑05‑13 19:29:16 | | 1.3.6.1.4.1.19376.1.8.1.2.3 |  |  Macroscopic Observation Section (2.0) Macroscopic Observation Section (2.0) | 2014‑05‑13 11:57:09 | | 1.3.6.1.4.1.19376.1.8.1.2.4 |  |  Microscopic Observation Section (2.0) Microscopic Observation Section (2.0) | 2014‑05‑13 14:25:17 | | 1.3.6.1.4.1.19376.1.8.1.2.5 |  |  Diagnostic Conclusion Section (2.0) Diagnostic Conclusion Section (2.0) | 2014‑05‑13 19:31:26 | | 1.3.6.1.4.1.19376.1.8.1.4.9 | Containment |  AP Observation Entry (2.0) AP Observation Entry (2.0) | 2014‑05‑14 17:09:54 | |  Circular reference found with 1.3.6.1.4.1.19376.1.8.1.4.9, please check Circular reference found with 1.3.6.1.4.1.19376.1.8.1.4.9, please check | | Uses | as | Name | Version |
|---|
| 2.16.840.1.113883.10.12.315 | Containment |  CDA Device CDA Device | 2005‑09‑07 | | 2.16.840.1.113883.10.12.313 | Containment |  CDA PlayingEntity CDA PlayingEntity | 2005‑09‑07 |
|
|
|---|
| Relationship | Adaptation: template 2.16.840.1.113883.10.12.321 (2005‑09‑07) |
|---|
| Example | | generated example | <templateId root="1.3.6.1.4.1.19376.1.8.1.4.7"/><time/><participantRole classCode="ROL">
<id root="1.2.3.999" extension="--example only--"/> <addr>addr</addr> <telecom value="tel:+1-12345678"/> <!-- choice: 0..1
element hl7:playingDevice containing template 2.16.840.1.113883.10.12.315 (dynamic)
element hl7:playingEntity containing template 2.16.840.1.113883.10.12.313 (dynamic)
-->
</participantRole> |
|
|
on Art-Decor
6.2.6.7 AP Anatomic Pathology Observation template – 1.3.6.1.4.1.19376.1.8.1.4.9
6.2.6.7.1 Definition and purpose
This Content Module is usable within a Problem Organizer.
The “AP Observation” generic template is usable for all AP observations, including those on findings from ancillary
techniques.
An AP Observation has a status and an effective time, may describe various participants (persons, devices, organizations), may have a number of additional properties (method,
interpretation, text), and may contain embedded images, comments, and sub-observations, which are also AP observations.
6.2.6.7.2 Specification and Example
| Id | 1.3.6.1.4.1.19376.1.8.1.4.9 | Effective Date | valid from 2014‑05‑14 17:09:54 |
|---|
| Status |  Draft Draft | Version Label | 2.0 |
|---|
| Name | APObservationEntry | Display Name | AP Observation Entry |
|---|
| Description | This content module is usable within a Problem organizer.
The “AP Observation” generic template is usable for all AP observations, including ancillary techniques.
An AP observation has a status and an effective time, may describe various participants (persons, devices, organizations), may have a number of additional properties (method, interpretation, text), and may contain embedded images, comments, and sub-observations, which are also AP observations.
|
|
| Context | Parent nodes of template element with id 1.3.6.1.4.1.19376.1.8.1.4.9 |
|---|
| Label | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation
|
|---|
| Classification | CDA Entry Level Template |
|---|
| Open/Closed | Open (other than defined elements are allowed) |
|---|
| Used by / Uses | | Used by 0 transactions and 9 templates, Uses 10 templates | | Used by | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.8.1.3.6 | Containment |  Problem Organizer (2.0) Problem Organizer (2.0) | 2015‑08‑13 10:24:55 | | 1.3.6.1.4.1.19376.1.3.10.3.1 |  |  Additional Specified Observation Section (2.0) Additional Specified Observation Section (2.0) | 2016‑11‑13 14:28:08 | | 1.3.6.1.4.1.19376.1.8.1.1.1 |  |  Anatomic Pathology Structured Report Content Module (2.0) Anatomic Pathology Structured Report Content Module (2.0) | 2014‑05‑13 11:57:57 | | 1.3.6.1.4.1.19376.1.8.1.2.1 |  |  Clinical Information Section (2.0) Clinical Information Section (2.0) | 2014‑05‑13 14:38:08 | | 1.3.6.1.4.1.19376.1.8.1.2.2 |  |  Intraoperative Observation Section (2.0) Intraoperative Observation Section (2.0) | 2014‑05‑13 19:29:16 | | 1.3.6.1.4.1.19376.1.8.1.2.3 |  |  Macroscopic Observation Section (2.0) Macroscopic Observation Section (2.0) | 2014‑05‑13 11:57:09 | | 1.3.6.1.4.1.19376.1.8.1.2.4 |  |  Microscopic Observation Section (2.0) Microscopic Observation Section (2.0) | 2014‑05‑13 14:25:17 | | 1.3.6.1.4.1.19376.1.8.1.2.5 |  |  Diagnostic Conclusion Section (2.0) Diagnostic Conclusion Section (2.0) | 2014‑05‑13 19:31:26 | | 1.3.6.1.4.1.19376.1.8.1.4.9 | Containment |  AP Observation Entry (2.0) AP Observation Entry (2.0) | 2014‑05‑14 17:09:54 | |  Circular reference found with 1.3.6.1.4.1.19376.1.8.1.4.9, please check Circular reference found with 1.3.6.1.4.1.19376.1.8.1.4.9, please check | | Uses | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.3.3.1.7 | Containment |  Laboratory Performer (2017) Laboratory Performer (2017) | 2008‑08‑08 | | 1.3.6.1.4.1.19376.1.8.1.4.2 | Containment |  CDA author IHE CDA author IHE | 2016‑06‑21 14:02:11 | | 1.3.6.1.4.1.19376.1.8.1.4.6 | Containment |  CDA Informant(Header&Body) APSR2 (2.0) CDA Informant(Header&Body) APSR2 (2.0) | 2016‑07‑08 11:22:58 | | 1.3.6.1.4.1.19376.1.8.1.4.7 | Containment |  Additional participant in an entry APSR (Body) Additional participant in an entry APSR (Body) | 2016‑07‑12 18:44:06 | | 1.3.6.1.4.1.19376.1.8.1.4.9 | Containment |  AP Observation Entry (2.0) AP Observation Entry (2.0) | 2014‑05‑14 17:09:54 | | 1.3.6.1.4.1.19376.1.8.1.4.10 | Containment |  Embedded Image IHE Embedded Image IHE | 2016‑06‑22 16:08:01 | | 2.16.840.1.113883.10.12.307 | Containment |  CDA RegionOfInterest CDA RegionOfInterest | 2005‑09‑07 | | 1.3.6.1.4.1.19376.1.5.3.1.4.2 | Containment |  IHE Comment Entry (2014) IHE Comment Entry (2014) | 2013‑12‑20 | | 1.3.6.1.4.1.19376.1.3.10.9.1 | Include |  X Specimen Identified X Specimen Identified | 2014‑12‑22 15:54:30 | | 2.16.840.1.113883.10.12.324 | Containment |  CDA Reference CDA Reference | 2005‑09‑07 |
|
|
|---|
| Relationship | Specialization: template 2.16.840.1.113883.10.12.303 (2005‑09‑07) |
|---|
| Example | | Observation example for use case #1, estrogen receptor | <observation classCode="OBS" moodCode="EVN" negationInd="false">
<templateId root="1.3.6.1.4.1.19376.1.8.1.4.9"/> <id root="1.2.3.999" extension="--example only--"/> <code code="16112-5" codeSystem="2.16.840.1.113883.6.1" displayName="Estrogen receptor [Interpretation] in Tissue"/> <text/> <statusCode code="completed"/> <effectiveTime>
<low value="20161129162112"/> </effectiveTime> <value xsi:type="CD" code="416053008" displayName="Estrogen receptor positive tumor (disorder)" codeSystem="2.16.840.1.113883.6.96"/> <methodCode code="0107" displayName="Microscopy" codeSystem="2.16.840.1.113883.5.84"/> <performer>
<!-- template 1.3.6.1.4.1.19376.1.3.3.1.7 'CDA Performer IHE (Body)' (dynamic) -->
</performer> <author>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.2 'CDA author' (dynamic) -->
</author> <informant>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.6 'CDA Informant(Body) APSR2' (dynamic) -->
</informant> <participant>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.7 'Additional participant in an entry APSR (Body)' (dynamic) -->
</participant> <entryRelationship xsi:type="" typeCode="COMP">
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.9 'AP Observation Entry' (dynamic) -->
</entryRelationship> <entryRelationship xsi:type="" typeCode="COMP">
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.10 'Embedded Image IHE' (dynamic) -->
</entryRelationship> <entryRelationship xsi:type="" typeCode="COMP">
<!-- template 2.16.840.1.113883.10.12.307 'CDA RegionOfInterest' (dynamic) -->
</entryRelationship> <!-- include template 1.3.6.1.4.1.19376.1.3.10.9.1 'X Specimen Identified' (dynamic) 0..* O -->
<reference>
<!-- template 2.16.840.1.113883.10.12.324 'CDA Reference' (dynamic) -->
</reference></observation> |
|
| Item | DT | Card | Conf | Description | Label |
|---|
| | 0 … * | R | | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | @classCode
|
| cs | 1 … 1 | F | OBS |  | @moodCode
|
| cs | 1 … 1 | F | EVN |  | @negationInd
|
| bl | 0 … 1 | | |  | hl7:templateId
|
| II | 1 … 1 | M | | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  |  | @root
|
| uid | 1 … 1 | F | 1.3.6.1.4.1.19376.1.8.1.4.9 |  | hl7:id
|
| II | 0 … * | R | | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | hl7:code
|
| CE (extensible) | 1 … 1 | M | The Anatomic pathology observation code should be taken from a reference terminology, preferably the LOINC terminology. National terminologies may be used. | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  |  | @code
|
| CONF | 1 … 1 | F | each_code_for_observable_entities_or_a_specific_procedure |  |  | @codeSystem
|
| 1 … 1 | F | 2.16.840.1.113883.6.1 (Logical Observation Identifier Names and Codes) |  |  | @codeSystemName
|
| 1 … 1 | F | LOINC |  |  | @displayName
|
| 1 … 1 | F | see_above | | | Example | <code code="59847-4" codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC" displayName="Histology and Behavior ICD-O-3"/> |  | hl7:text
|
| ED | 0 … 1 | R | Narrative text about the observation | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | hl7:statusCode
|
| CS (required) | 1 … 1 | M | The observation statusCode is “completed” if the observation was actually performed and has produced a result in the
value
element. In other cases the status of the intended observation is “aborted” and the result will never come. | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation | | | CONF | The value of @code shall be drawn from value set 1.3.6.1.4.1.19376.1.3.11.2 (DYNAMIC) | Error: Cannot find value set "1.3.6.1.4.1.19376.1.3.11.2" |
|
|  | hl7:effectiveTime
|
| IVL_TS | 1 … 1 | M | Date and time the observation has been made
| PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | hl7:value
|
| ANY | 0 … * | R | Observation values using the appropriate data type.
Numeric results use data type PQ, which includes the unit. The result is absent in case of ‘aborted’ observation.
| PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation | | | Constraint | The default data type, cardinalities and value set for the <value> element are dependant on the type of observation. | | | CONF | | The value of @code shall be drawn from value set 1.3.6.1.4.1.19376.1.3.11.11 AP Observation (2015‑11‑22 12:20:34) |
| | | Example | for observation on tumor type <value code="8500/3" codeSystem="2.16.840.1.113883.6.43.1" codeSystemName="ICD-O-3" displayName="Invasive carcinoma of the breast, no special type"/> |  | hl7:interpretationCode
|
| CE (extensible) | 0 … 1 | R | One or more codes interpreting the result, expressed with ObservationInterpretation vocabulary (e.g., H = high, L = low).
This element may be coded with other values than those of the ObservationInterpretation vocabulary, given that the coding strength is CWE (coded with exceptions).
| PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation | | | CONF | | The value of @code should be drawn from value set 2.16.840.1.113883.1.11.78 ObservationInterpretation (2014‑03‑26) |
|  | hl7:methodCode
|
| CE (extensible) | 0 … 1 | R | | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation | | | CONF | | The value of @code should be drawn from value set 2.16.840.1.113883.1.11.14079 ObservationMethod (2014‑03‑26) |
|  | hl7:performer
|
| II | 0 … 1 | C | Performing lab
Source: PaLM TF-3: 6.3.2.20
Contains 1.3.6.1.4.1.19376.1.3.3.1.7 Laboratory Performer (2008‑08‑08) | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | where [hl7:templateId [@root='1.3.6.1.4.1.19376.1.3.3.1.7']] |
| | | | Constraint | The performing laboratory is present at this level only if this particular observation was performed by a (subcontractor) laboratory distinct from the one issuing the rest of the observations in this organizer.
|  | hl7:author
|
| II | 0 … * | C | Author
Source: PaLM TF Suppl. APSR 2.0-3:
6.3.6.2
Contains 1.3.6.1.4.1.19376.1.8.1.4.2 CDA author IHE (2016‑06‑21 14:02:11) | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | where [hl7:author [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.2']]] |
| |  | hl7:informant
|
| II | 0 … * | R | Informant
Source: PaLM TF Suppl. APSR 2.0-3
: 6.3.6.5
Contains 1.3.6.1.4.1.19376.1.8.1.4.6 CDA Informant(Header&Body) APSR2 (2016‑07‑08 11:22:58) | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | where [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.6']] |
| |  | hl7:participant
|
| II | 0 … * | R | Additional participants
Source: PaLM TF Suppl. APSR 2.0-3
: 6.3.6.6
Contains 1.3.6.1.4.1.19376.1.8.1.4.7 Additional participant in an entry APSR (Body) (2016‑07‑12 18:44:06) | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | where [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.7']] |
| |  | hl7:entryRelationship
|
| | 0 … * | R | Sub-Observation
The result obtained for an observation may lead to an additional AP observation to refine this result. This sub-observation is again an Anatomic Pathology Observation.
Source: Source: PaLM TF Suppl. APSR 2.0-3
: 6.3.6.7
Contains 1.3.6.1.4.1.19376.1.8.1.4.9 AP Observation Entry (2014‑05‑14 17:09:54) | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | where [@typeCode='COMP'] [hl7:observation [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.9']]] |
| |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP |  | hl7:entryRelationship
|
| | 0 … * | R | Embedded image.
This observation may carry an illustrative image, either directly embedded or encapsulated within a region of interest.
Source: PaLM TF Suppl. APSR 2.0-3
: 6.3.6.8
Contains 1.3.6.1.4.1.19376.1.8.1.4.10 Embedded Image IHE (2016‑06‑22 16:08:01) | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | where [@typeCode='COMP'] [hl7:observationMedia [hl7:templateId [@root='1.3.6.1.4.1.19376.1.8.1.4.10']]] |
| |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP |  | hl7:entryRelationship
|
| | 0 … * | R | Region of Interest
Contains 2.16.840.1.113883.10.12.307 CDA RegionOfInterest (2005‑09‑07) | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | where [@typeCode='COMP'] [hl7:regionOfInterest [hl7:templateId [@root='2.16.840.1.113883.10.12.307']]] |
| |  |  | @typeCode
|
| cs | 1 … 1 | F | COMP | | | Constraint | This observation may carry an illustrative image, either directly embedded or encapsulated within a region of interest.
In the latter case by an entryRelationship @typeCode="SUBJ" |  | hl7:entryRelationship
|
| | 0 … * | R | Annotation comment
Contains 1.3.6.1.4.1.19376.1.5.3.1.4.2 IHE Comment Entry (2013‑12‑20) | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |  | where [hl7:act [hl7:templateId [@root='2.16.840.1.113883.10.20.1.40'] and hl7:templateId [@root='1.3.6.1.4.1.19376.1.5.3.1.4.2']]] |
| |  |  | @typeCode
|
| cs | 0 … 1 | F | COMP | | Included | 1 … * | M | from 1.3.6.1.4.1.19376.1.3.10.9.1 X Specimen Identified (2014‑12‑22 15:54:30)
Specimen identification
| | | Example | Example for specimen referencing <specimen>
<!-- which specimen is used for this observation -->
<specimenRole>
<id root="1.3.6.1.4.1.19376.1.8.1.4.999999" extension="slide_A_1_PR"/> </specimenRole></specimen> |  | hl7:specimen
|
| | 1 … * | M | Required in XD-LAB when more than one specimen is documented at this level. Always required in APSR.
| PaLM Suppl. APSR 2.0‑3: 6.3.6.9 X Specimen identified |  |  | @typeCode
|
| cs | 0 … 1 | F | SPC |  |  | hl7:specimenRole
|
| | 1 … 1 | M | | PaLM Suppl. APSR 2.0‑3: 6.3.6.9 X Specimen identified | | cs | 0 … 1 | F | SPEC | | II | 1 … 1 | R | Specimen ID, coming from the LIS | PaLM Suppl. APSR 2.0‑3: 6.3.6.9 X Specimen identified |  | hl7:reference
|
| | 0 … * | R | Reference to an external document, or to external observations, e.g. concerning molecular pathology or genetic testing report
Contains 2.16.840.1.113883.10.12.324 CDA Reference (2005‑09‑07) | PaLM TF Suppl. APSR 2.0‑3: 6.3.6.7 AP observation |
|
on Art-Decor
6.2.6.8 Embedded Image – 1.3.6.1.4.1.19376.1.8.1.4.10
6.2.6.8.1 Definition and purpose
This Content Module is usable within an <entry> element, in relationship with a
display anchor carried in the referencedObject attribute of a <renderMultimedia>
element in the <text> element of the <section> holding this <entry>.
The <observationMedia> element carries an image, embedded in B64. This element may be standalone, or encapsulated within a <regionOfInterest> element which defines an overlay
shape to focus on a part of the image.
This <observationMedia> element embeds the image binary data, encoded in B64.
6.2.6.8.2 Specification and Example
on Art-Decor
6.2.6.9 X Specimen Identified - 1.3.6.1.4.1.19376.1.3.10.9.1
 |
This is an addendum to the reference text of APSR 2.0 GH |
6.2.6.9.1 Definition and purpose
This Specimen Identification <entry> provides the machine-readable links between any type of observation or embedded image or containers to the specimen, from which this observation or image is obtained.
It is required when more than one specimen is documented at this level.
It is only used in PaLM templates for Problem Organizer, Observations, Embedded images, and Containers in Specimen Procedure Steps.
6.2.6.9.2 Specification and Example
on Art-Decor
6.2.6.10 UICC/AJCC TNM Staging and Grading - 1.3.6.1.4.1.19376.1.3.10.4.2
 |
This is an addendum to the reference text of APSR 2.0 GH |
6.2.6.10.1 Definition and purpose
The UICC/AJCC TNM <entry> Content Modul contains in machine-readable form all the information concerning a TNM formula for a problem investigated. It is a constraint version of an AP Generic observation <entry> Content Module. It is usable within a Problem Organizer <entry> Content Module only.
This Content Module structures the machine-readable data, which characterize the staging and grading of a malignant Tumor according the UICC/AJCC regulations for the TNM system. A series of supporting templates is used for all the detailed descriptions of the elements of the TNM system.
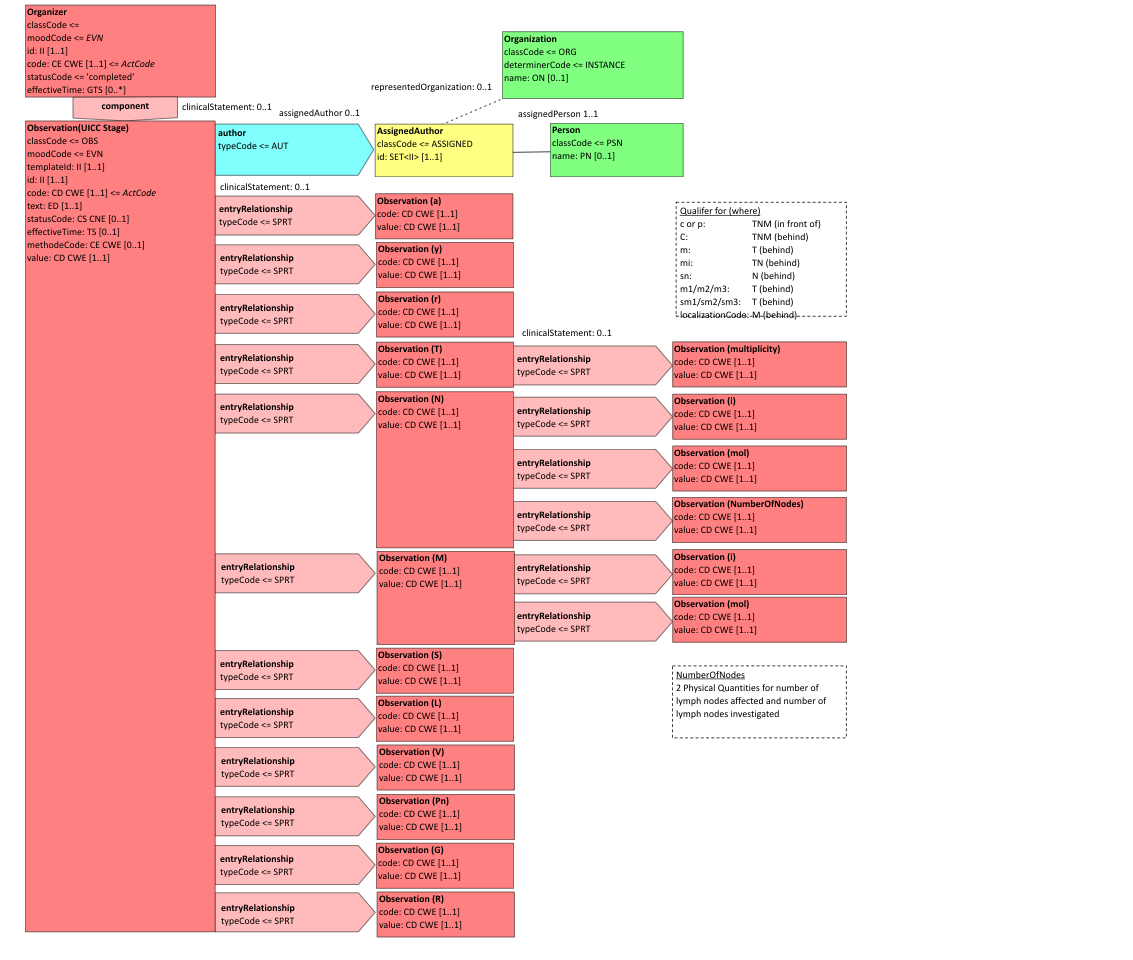
Figure 6.2.6.10.1-1 CDA-RMIM of the UICC/AJCC TNM <entry>
6.2.6.10.2 Specification and Example
| Id | 1.3.6.1.4.1.19376.1.3.10.4.2 | Effective Date | valid from 2014‑05‑13 15:45:13 |
|---|
| Status |  Draft Draft | Version Label | 2.0 |
|---|
| Name | TNMStageObservation | Display Name | TNM Stage Observation |
|---|
| Description | Template CDA Observation (prototype, directly derived from POCD_RM000040 MIF)
TNM stage with supporting categories |
|---|
| Context | Parent nodes of template element with id 1.3.6.1.4.1.19376.1.3.10.4.2 |
|---|
| Label | PaLM Suppl. APSR 2.0‑3: 6.3.6.10 TNM
|
|---|
| Classification | CDA Entry Level Template |
|---|
| Open/Closed | Open (other than defined elements are allowed) |
|---|
| Used by / Uses | | Used by 0 transactions and 1 template, Uses 17 templates | | Used by | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.3.10.4.1 | Containment |  Specimen Procedure Step (1.0) Specimen Procedure Step (1.0) | 2014‑07‑29 16:02:02 | | Uses | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.3.3.1.7 | Containment |  Laboratory Performer (2017) Laboratory Performer (2017) | 2008‑08‑08 | | 1.3.6.1.4.1.19376.1.8.1.4.2 | Containment |  CDA author IHE CDA author IHE | 2016‑06‑21 14:02:11 | | 1.3.6.1.4.1.19376.1.8.1.4.6 | Containment |  CDA Informant(Header&Body) APSR2 (2.0) CDA Informant(Header&Body) APSR2 (2.0) | 2016‑07‑08 11:22:58 | | 1.3.6.1.4.1.19376.1.8.1.4.7 | Containment |  Additional participant in an entry APSR (Body) Additional participant in an entry APSR (Body) | 2016‑07‑12 18:44:06 | | 1.3.6.1.4.1.19376.1.3.10.9.1 | Include |  X Specimen Identified X Specimen Identified | 2014‑12‑22 15:54:30 | | 1.3.6.1.4.1.19376.1.3.10.9.32 | Containment |  TNM y (2.0) TNM y (2.0) | 2015‑06‑22 17:28:17 | | 1.3.6.1.4.1.19376.1.3.10.9.30 | Containment |  TNM a (2.0) TNM a (2.0) | 2015‑06‑22 15:13:46 | | 1.3.6.1.4.1.19376.1.3.10.9.31 | Containment |  TNM r (2.0) TNM r (2.0) | 2015‑06‑22 17:38:42 | | 1.3.6.1.4.1.19376.1.3.10.9.25 | Containment |  TNM T-Observation (2.0) TNM T-Observation (2.0) | 2014‑12‑02 15:54:17 | | 1.3.6.1.4.1.19376.1.3.10.9.26 | Containment |  TNM N-Observation (2.0) TNM N-Observation (2.0) | 2014‑12‑02 16:34:50 | | 1.3.6.1.4.1.19376.1.3.10.9.27 | Containment |  TNM M-Observation (2.0) TNM M-Observation (2.0) | 2014‑12‑02 16:32:30 | | 1.3.6.1.4.1.19376.1.3.10.9.33 | Containment |  TNM Serum tumor markers (2.0) TNM Serum tumor markers (2.0) | 2015‑11‑06 14:28:44 | | 1.3.6.1.4.1.19376.1.3.10.9.34 | Containment |  TNM Lymphatic Invasion (2.0) TNM Lymphatic Invasion (2.0) | 2015‑11‑16 14:01:58 | | 1.3.6.1.4.1.19376.1.3.10.9.35 | Containment |  TNM Venous Invasion (2.0) TNM Venous Invasion (2.0) | 2015‑11‑16 13:40:28 | | 1.3.6.1.4.1.19376.1.3.10.9.36 | Containment |  TNM Perineural Invasion (2.0) TNM Perineural Invasion (2.0) | 2015‑11‑11 16:13:40 | | 1.3.6.1.4.1.19376.1.3.10.9.28 | Containment |  TNM Grading (2.0) TNM Grading (2.0) | 2015‑11‑15 13:01:18 | | 1.3.6.1.4.1.19376.1.3.10.9.29 | Containment |  TNM R-status (2.0) TNM R-status (2.0) | 2015‑06‑30 13:38:30 |
|
|
|---|
| Relationship | Specialization: template 1.3.6.1.4.1.19376.1.8.1.4.9 (2014‑05‑14 17:09:54) |
|---|
| Example | | Generated example | <observation classCode="OBS" moodCode="ENV" negationInd="false">
<templateId root="1.3.6.1.4.1.19376.1.3.10.4.2"/> <id root="1.2.3.999" extension="--example only--"/> <code code="21902-2" codeSystem="2.16.840.1.113883.6.1"/> <text/> <statusCode code="completed"/> <effectiveTime>
<low value="20170712152253"/> </effectiveTime> <value xsi:type="CD" code="IIA" displayName="stage IIA" codeSystem="2.16.840.1.113883.15.6"/> <performer>
<!-- template 1.3.6.1.4.1.19376.1.3.3.1.7 'Laboratory Performer' (2008-08-08T00:00:00) -->
</performer> <author>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.2 'CDA author IHE' (2016-06-21T14:02:11) -->
</author> <informant>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.6 'CDA Informant(Header&Body) APSR2' (2016-07-08T11:22:58) -->
</informant> <participant>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.7 'Additional participant in an entry APSR (Body)' (2016-07-12T18:44:06) -->
</participant> <!-- include template 1.3.6.1.4.1.19376.1.3.10.9.1 'X Specimen Identified' (2014-12-22T15:54:30) 1..* M -->
<entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.32 'TNM y' (2015-06-22T17:28:17) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.30 'TNM a ' (2015-06-22T15:13:46) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.31 'TNM r' (2015-06-22T17:38:42) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.25 'TNM T-Observation' (2014-12-02T15:54:17) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.26 'TNM N-Observation' (2014-12-02T16:34:50) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.27 'TNM M-Observation' (2014-12-02T16:32:30) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.33 'TNM Serum tumor markers' (2015-11-06T14:28:44) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.34 'TNM Lymphatic Invasion' (2015-11-16T14:01:58) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.35 'TNM Venous Invasion' (2015-11-16T13:40:28) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.36 'TNM Perineural Invasion' (2015-11-11T16:13:40) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.28 'TNM Grading' (2015-11-15T13:01:18) -->
</entryRelationship> <entryRelationship>
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.29 'TNM R-status' (2015-06-30T13:38:30) -->
</entryRelationship></observation> |
|
|
on Art-Decor
6.2.6.11 ICD-O-3 Typing and Grading - 1.3.6.1.4.1.19376.1.3.10.4.3
 |
This is an addendum to the reference text of APSR 2.0 GH |
6.2.6.11.1 Definition and purpose
The ICD-O-3 Typing and Grading<entry> Content Modul contains in machine-readable form all the information concerning ICD-O-3 Typing and Grading for a problem investigated. It is a constraint version of an AP Generic observation <entry> Content Module. It is usable within a Problem Organizer <entry> Content Module only.
This Content Module structures the machine-readable data, which characterize the typing and grading of a tumor or a systemic malignancy according the WHO regulations for the ICD-O-3 system. A series of supporting templates is used for all the detailed descriptions of the elements of the ICD-O-3 system.
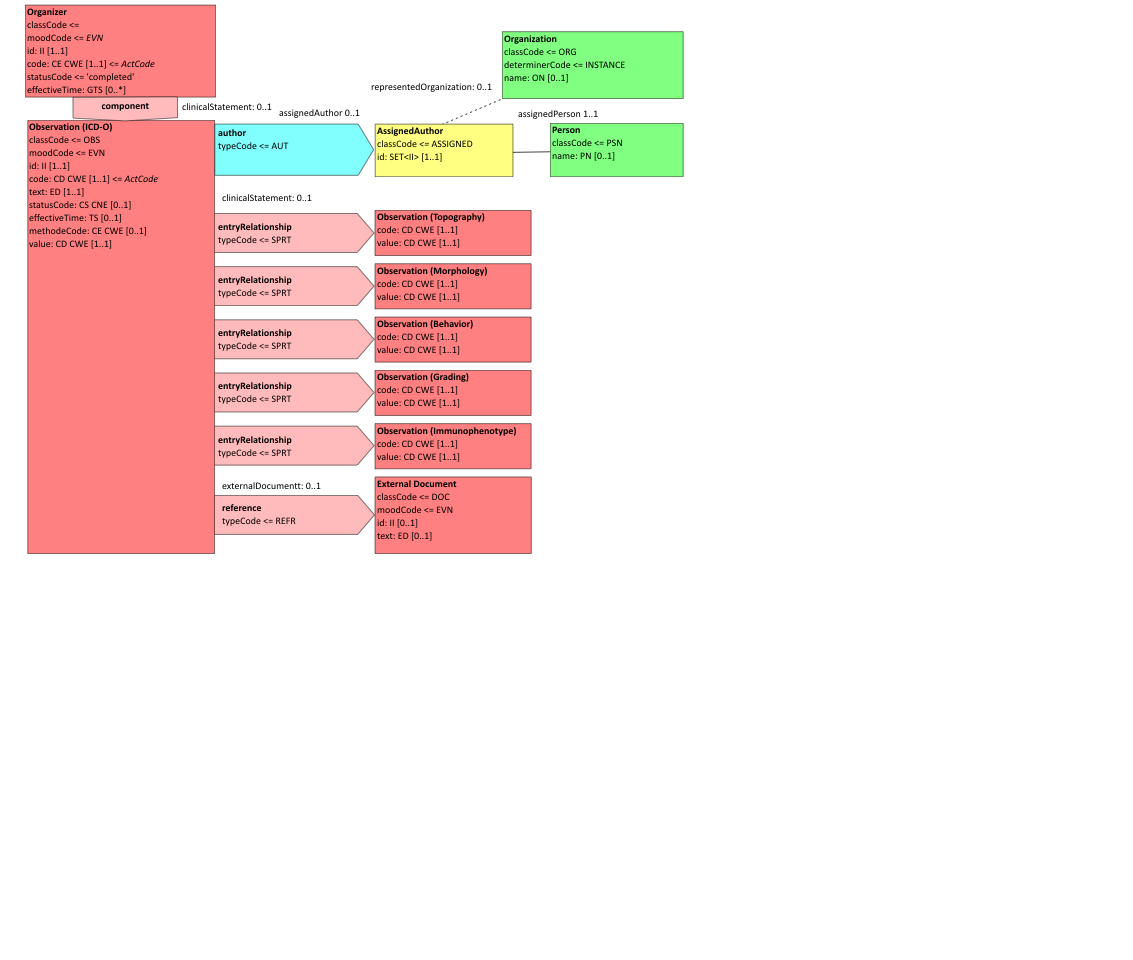
Figure 6.2.6.11.1-1 CDA-RMIM of the ICD-O-3 <entry>
6.2.6.11.2 Specification and Example
| Id | 1.3.6.1.4.1.19376.1.3.10.4.3 | Effective Date | valid from 2015‑11‑29 17:03:18 |
|---|
| Status |  Draft Draft | Version Label | 2.0 |
|---|
| Name | ICD-O-3TypingGrading | Display Name | ICD-O-3 Typing and Grading Observation |
|---|
| Description | Template CDA Observation (prototype, directly derived from POCD_RM000040 MIF)
Entry template for observation on ICD-O-3 Typing and Grading |
|---|
| Context | Parent nodes of template element with id 1.3.6.1.4.1.19376.1.3.10.4.3 |
|---|
| Label | PaLM Suppl. APSR 2.0‑3: 6.3.6.11 ICD‑O‑3
|
|---|
| Classification | CDA Entry Level Template |
|---|
| Open/Closed | Open (other than defined elements are allowed) |
|---|
| Used by / Uses | | Used by 0 transactions and 0 templates, Uses 9 templates | | Uses | as | Name | Version |
|---|
| 1.3.6.1.4.1.19376.1.3.3.1.7 | Containment |  Laboratory Performer (2017) Laboratory Performer (2017) | 2008‑08‑08 | | 1.3.6.1.4.1.19376.1.8.1.4.2 | Containment |  CDA author IHE CDA author IHE | 2016‑06‑21 14:02:11 | | 1.3.6.1.4.1.19376.1.8.1.4.6 | Containment |  CDA Informant(Header&Body) APSR2 (2.0) CDA Informant(Header&Body) APSR2 (2.0) | 2016‑07‑08 11:22:58 | | 1.3.6.1.4.1.19376.1.8.1.4.7 | Containment |  Additional participant in an entry APSR (Body) Additional participant in an entry APSR (Body) | 2016‑07‑12 18:44:06 | | 1.3.6.1.4.1.19376.1.3.10.9.1 | Include |  X Specimen Identified X Specimen Identified | 2014‑12‑22 15:54:30 | | 1.3.6.1.4.1.19376.1.3.10.9.38 | Containment |  ICD-O-3 Behavior (2.0) ICD-O-3 Behavior (2.0) | 2015‑12‑03 09:11:54 | | 1.3.6.1.4.1.19376.1.3.10.9.39 | Containment |  ICD-O-3 Differentiation (2.0) ICD-O-3 Differentiation (2.0) | 2015‑12‑09 17:12:30 | | 1.3.6.1.4.1.19376.1.3.10.4.4 | Containment |  Assessment Scales Observation for Scoring Systems APSR2 (2.0) Assessment Scales Observation for Scoring Systems APSR2 (2.0) | 2016‑10‑06 13:12:00 | | 2.16.840.1.113883.10.12.324 | Containment |  CDA Reference CDA Reference | 2005‑09‑07 |
|
|
|---|
| Relationship | Specialization: template 1.3.6.1.4.1.19376.1.8.1.4.9 (2014‑05‑14 17:09:54) |
|---|
| Example | | example for use case #1 | <observation classCode="OBS" moodCode="EVN" negationInd="false">
<templateId root="1.3.6.1.4.1.19376.1.3.10.4.3"/> <id root="1.3.6.1.4.1.19376.1.8.9.1" extension="A7102400008_ICDO"/> <code code="31205-8" codeSystem="2.16.840.1.113883.6.1" displayName="Histology ICD-O-3 Cancer"/> <statusCode code="completed"/> <effectiveTime>
<low value="201001041405-0500"/> </effectiveTime> <value xsi:type="CD" code="8500/3" codeSystem="2.16.840.1.113883.6.43.1"/> <author>
<!-- template 1.3.6.1.4.1.19376.1.8.1.4.2 'CDA author IHE' (2016-06-21T14:02:11) -->
</author> <!-- include template 1.3.6.1.4.1.19376.1.3.10.9.1 'X Specimen Identified' (2014-12-22T15:54:30) 1..* R -->
<specimen typeCode="SPC">
<specimenRole classCode="SPEC">
<id root="1.3.6.1.4.1.19376.1.8.9.1" extension="A7102400008_slide_A1_HE"/> </specimenRole> </specimen> <entryRelationship typeCode="SPRT">
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.38 'ICD-O-3 Behavior' (2015-12-03T09:11:54), not used in use case #1 -->
</entryRelationship> <entryRelationship typeCode="SPRT">
<!-- template 1.3.6.1.4.1.19376.1.3.10.9.39 'ICD-O-3 Differentiation' (2015-12-09T17:12:30) -->
</entryRelationship> <entryRelationship typeCode="COMP">
<!-- template 1.3.6.1.4.1.19376.1.3.10.4.4 'Assessment Scales Observation for Scoring Systems APSR2' (2016-10-06T13:12:00) -->
</entryRelationship> <reference>
<!-- template 2.16.840.1.113883.10.12.324 'CDA Reference' (2005-09-07T00:00:00) -->
</reference></observation> |
|
|
on Art-Decor
6.2.6.12 Assessment Scales for Scoring systems - 1.3.6.1.4.1.19376.1.3.10.4.4
 |
This is an addendum to the reference text of APSR 2.0 GH |
6.2.6.12.1 Definition and purpose
The Assessment Scales <entry> Content Modul contains in machine-readable form all the information concerning (semi)quantitative scoring systems often used for describing a tumor grading for a problem investigated. It is a constraint version of an AP Generic observation <entry> Content Module. It is usable within the ICD-O-3 Typing and Grading <entry> or within a Problem Organizer <entry> Content Module.
This Content Module structures the machine-readable data, which characterize the grading components of a tumor or a systemic disease according specific regulations.
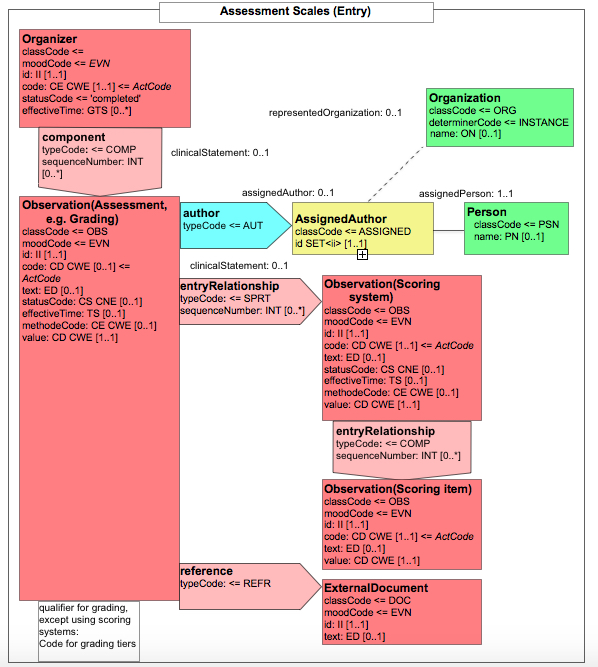
Figure 6.2.6.12.1-1 CDA-RMIM of an Assessment Scales <entry>
6.2.6.12.2 Specification and Example
on Art-Decor
VOLUME 4 - VALUE SETS
Generic AP Observation Codes 1.3.6.1.4.1.19376.1.3.11.11
| Id | 1.3.6.1.4.1.19376.1.3.11.11 | Effective Date | valid from 2015‑11‑22 12:20:34 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | AP-Observation | Display Name | AP Observation |
|---|
| Description | Generic codes for AP Observations of all kind, including results of ancillary techniques (immunohistochemistry, in-situ-hybridization, other molecular methods) |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
A valid code from one of the 12 code systems:| Code System Name | Code System Id | Code System Version | Flexibility | | Logical Observation Identifier Names and Codes | 2.16.840.1.113883.6.1 | | DYNAMIC | | SNOMED Clinical Terms | 2.16.840.1.113883.6.96 | | DYNAMIC | | International Classification of Diseases for Oncology, version 3. | 2.16.840.1.113883.6.43.1 | | DYNAMIC | | ICD10 | 2.16.840.1.113883.6.3 | | DYNAMIC | | TNM Edition8 UICC | 2.16.840.1.113883.15.16 | | DYNAMIC | | TNM Edition7 UICC | 2.16.840.1.113883.15.6 | | DYNAMIC | | TNM Edition6 UICC | 2.16.840.1.113883.15.7 | | DYNAMIC | | TNM Edition5 UICC | 2.16.840.1.113883.15.8 | | DYNAMIC | | Unified Code for Units of Measure | 2.16.840.1.113883.6.8 | | DYNAMIC | | Online Mendelian Inheritance in Man 1993 | 2.16.840.1.113883.6.174 | | DYNAMIC | | DKG Coding scheme | 1.2.276.0.76.3.1.131.1.5.1 | | DYNAMIC | | localization codes for distant metastases | 1.2.276.0.76.5.401 | | DYNAMIC |
|
on Art-Decor
Problem type 1.3.6.1.4.1.19376.1.3.11.7
| Id | 1.3.6.1.4.1.19376.1.3.11.7 | Effective Date | valid from 2016‑07‑11 09:52:19 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | ProblemType | Display Name | Problem Type |
|---|
| Description | Values for the problem under investigation |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
A valid code from the code system:| Code System Name | Code System Id | Code System Version | | ICD10 | 2.16.840.1.113883.6.3 | |
|
| Or one of the following: |
| 4 Source Code Systems | 2.16.840.1.113883.6.3 - ICD10 2.16.840.1.113883.6.96 - SNOMED Clinical Terms 2.16.840.1.113883.5.6 - ActClass 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | 115597007 | Description of specimen character (procedure) | SNOMED Clinical Terms | | 0‑L | 128462008 | Secondary malignant neoplastic disease (disorder) | SNOMED Clinical Terms | | 0‑L | 367651003 | Malignant neoplasm of primary, secondary, or uncertain origin (morphologic abnormality) | SNOMED Clinical Terms | | 0‑L | SPCOBS | specimen observation | ActClass | | 0‑L | 3898006 | Neoplasm, benign (morphologic abnormality) | SNOMED Clinical Terms | | 0‑L | 109355002 | Carcinoma in situ (disorder) | SNOMED Clinical Terms | | 0‑L | 23583003 | Inflammation (morphologic abnormality) | SNOMED Clinical Terms | | 0‑L | 33359002 | Degeneration (morphologic abnormality) | SNOMED Clinical Terms | | 0‑L | 49601007 | Disorder of cardiovascular system (disorder) | SNOMED Clinical Terms | | 0‑L | ASKU | asked but unknown | Null Flavor |
|
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
Container Entity Class Type 1.3.6.1.4.1.19376.1.3.11.8
| Id | 1.3.6.1.4.1.19376.1.3.11.8 | Effective Date | valid from 2016‑09‑08 11:55:11 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | ContainerEntityClassTypePaLM | Display Name | ContainerEntityClassTypePaLM |
|---|
| Description | Types of Containers and their additives in Anatomic Pathology |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.6.96 - SNOMED Clinical Terms 1.2.840.10008.2.16.4 - DICOM Controlled Terminology |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | 434746001 | Specimen vial (physical object) | SNOMED Clinical Terms | | 0‑L | 434464009 | Tissue cassette (physical object) | SNOMED Clinical Terms | | 0‑L | 434708008 | Tissue cassette for microarray (physical object) | SNOMED Clinical Terms | | 0‑L | 433466003 | Microscope slide (physical object) | SNOMED Clinical Terms | | 0‑S | 433453003 | Specimen container component (physical object) | SNOMED Clinical Terms | | 1‑S | 430863003 | Tissue embedding medium (substance) | SNOMED Clinical Terms | | 2‑L | 311731000 | Paraffin wax (substance) | SNOMED Clinical Terms | | 2‑L | 433469005 | Frozen section embedding medium (substance) | SNOMED Clinical Terms | | 2‑L | 61088005 | Plastic (substance) | SNOMED Clinical Terms | | 2‑L | 10249006 | Agar (substance) | SNOMED Clinical Terms | | 2‑L | 65345002 | Epoxy resin (substance) | SNOMED Clinical Terms | | 2‑L | 427811002 | Polymethyl methacrylate (substance) | SNOMED Clinical Terms | | 1‑L | 433472003 | Microscope slide coverslip (physical object) | SNOMED Clinical Terms | | 1‑L | 430862008 | Microscope slide mounting medium (substance) | SNOMED Clinical Terms | | 0‑S | CID8101 | Container type | DICOM Controlled Terminology | | 1‑L | A-01024 | Specimen vial | DICOM Controlled Terminology | | 1‑L | A-0101B | Microscope slide | DICOM Controlled Terminology | | 1‑L | A-01023 | Specimen container | DICOM Controlled Terminology | | 1‑L | A-01021 | Electron microscopy grid | DICOM Controlled Terminology | | 1‑L | A-01025 | Specimen well | DICOM Controlled Terminology | | 0‑S | CID8114 | Fixatives | DICOM Controlled Terminology | | 0‑S | CID8102 | Container Component Types | DICOM Controlled Terminology | | 0‑S | CID8115 | Specimen Embedding Media | DICOM Controlled Terminology |
|
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
Procedure (target) site 1.3.6.1.4.1.19376.1.3.11.9
| Id | 1.3.6.1.4.1.19376.1.3.11.9 | Effective Date | valid from 2016‑06‑01 18:46:15 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | ProcedureSite | Display Name | Procedure Site |
|---|
| Description | Target sites of specimen processing procedures |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.6.96 - SNOMED Clinical Terms 1.2.840.10008.2.16.4 - DICOM Controlled Terminology |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | 309050000 | Body substance sample | SNOMED Clinical Terms | all children of "Body substance sample" | | 0‑L | 309051001 | Body fluid sample | SNOMED Clinical Terms | | | 0‑S | 430856003 | Tissue section (specimen) | SNOMED Clinical Terms | | | 1‑L | 441652008 | Formalin-fixed paraffin-embedded tissue specimen | SNOMED Clinical Terms | | | 1‑L | 16214131000119104 | Frozen tissue section sample (specimen) | SNOMED Clinical Terms | | | 0‑S | CID8103 | Anatomic Pathology Specimen Types | DICOM Controlled Terminology | | | 1‑L | G-843A | Gross specimen | DICOM Controlled Terminology | | | 1‑L | G-843B | Core sample of tissue block | DICOM Controlled Terminology | | | 1‑L | G-843C | Tissue spot | DICOM Controlled Terminology | | | 1‑L | G-803C | Smear sample | DICOM Controlled Terminology | | | 1‑L | T-1A404 | Touch preparation cytologic material | DICOM Controlled Terminology | | | 1‑L | T-1A403 | Liquid based cytologic material | DICOM Controlled Terminology | | | 1‑L | G-8003 | Aspirate | DICOM Controlled Terminology | | | 0‑L | 48469005 | Cytologic material (specimen) | SNOMED Clinical Terms | |
|
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
Specimen collection and processing 1.3.6.1.4.1.19376.1.3.11.10
| Id | 1.3.6.1.4.1.19376.1.3.11.10 | Effective Date | valid from 2016‑05‑31 15:09:59 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | SpecimenCollectionAndProcessing | Display Name | Specimen Collection and Processing |
|---|
| Description | Mixed Value set for Specimen collection and Processing |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
| 5 Source Code Systems | 2.16.840.1.113883.5.6 - ActClass 2.16.840.1.113883.6.96 - SNOMED Clinical Terms 1.2.276.0.76.5.464 1.2.840.10008.2.16.4 - DICOM Controlled Terminology 2.16.840.1.113883.6.4 - International Classification of Diseases, 10th Revision, Procedure Coding System (ICD-10-PCS) |
|---|
| Level/ Type | Code | Display Name | Code System | Designations |
|---|
| 0‑S | SPECCOLLECT | Specimen collection | ActClass | | | 1‑S | 17636008 | Specimen collection (procedure) | SNOMED Clinical Terms | | | 2‑L | 48635004 | Fine needle biopsy (procedure) | SNOMED Clinical Terms | | | 2‑S | 86273004 | Biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 439336003 | Brush biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 53767003 | Endoscopic biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 8889005 | Excisional biopsy (procedure) | SNOMED Clinical Terms | | | 3‑S | 277590007 | Imaging guided biopsy (procedure) | SNOMED Clinical Terms | | | 4‑L | 442787002 | Fine needle aspiration biopsy using imaging guidance (procedure) | SNOMED Clinical Terms | | | 4‑L | 277592004 | Magnetic resonance imaging guided biopsy (procedure) | SNOMED Clinical Terms | | | 4‑L | 277667006 | Ultrasound guided biopsy (procedure) | SNOMED Clinical Terms | | | 4‑L | 277666002 | X-ray guided biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 45681003 | Staging operation involving incision, exploration and biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 70871006 | Incisional biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 129249002 | Needle biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 119283008 | Open biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 68660007 | Punch biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 72342005 | Shave biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 274330002 | Surgical biopsy (procedure) | SNOMED Clinical Terms | | | 3‑L | 50590007 | Trephine biopsy (procedure) | SNOMED Clinical Terms | | | 2‑S | 65801008 | Excision (procedure) | SNOMED Clinical Terms | | | 3‑L | 81723002 | Amputation (procedure) | SNOMED Clinical Terms | | | 3‑L | 86743009 | Local excision (procedure) | SNOMED Clinical Terms | | | 3‑L | 125571002 | Lobectomy (procedure) | SNOMED Clinical Terms | | | 3‑L | 26007001 | Hemi-excision (procedure) | SNOMED Clinical Terms | | | 3‑L | 38829003 | Partial excision (procedure) | SNOMED Clinical Terms | | | 3‑L | 89540006 | Segmental excision and ligation (procedure) | SNOMED Clinical Terms | | | 3‑L | 65854006 | Reexcision (procedure) | SNOMED Clinical Terms | | | 3‑S | 62141006 | Radical excision (procedure) | SNOMED Clinical Terms | | | 4‑L | 88088007 | Radical excision with lymph node dissection (procedure) | SNOMED Clinical Terms | | | 3‑L | 79095000 | Complete excision of organ (procedure) | SNOMED Clinical Terms | | | 3‑L | 370612006 | Excision of neoplasm (procedure) | SNOMED Clinical Terms | | | 3‑L | 20418004 | Wedge resection (procedure) | SNOMED Clinical Terms | | | 2‑L | 56757003 | Scraping (procedure) | SNOMED Clinical Terms | | | 1‑L | 1-40...1-49 | Biopsies without incision | 1.2.276.0.76.5.464 | | | 1‑L | 1-50...1-58 | Biopsies with incision | 1.2.276.0.76.5.464 | | | 1‑L | 5-01...5-09 | Surgical measures | 1.2.276.0.76.5.464 | | | 1‑L | 1-10...1-99 | Diagnostic measures | 1.2.276.0.76.5.464 | | | 1‑S | CID8109 | all children of Specimen Collection Procedure | DICOM Controlled Terminology | | | 1‑S | 00...0Y | all children of 0 | International Classification of Diseases, 10th Revision, Procedure Coding System (ICD-10-PCS) | | | 0‑S | SPCTRT | Specimen treatment | ActClass | | | 1‑S | CID8110 | all children of Specimen Sampling Procedures | DICOM Controlled Terminology | | | 1‑S | CID8111 | all children of Specimen Preparation Procedure | DICOM Controlled Terminology | | | 1‑S | CID8112 | all children of Specimen Stains | DICOM Controlled Terminology | | | 1‑S | CID8113 | all children of Specimen Preparation Steps | DICOM Controlled Terminology | | | 1‑S | CID8114 | all children of Specimen Fixatives | DICOM Controlled Terminology | | | 1‑S | 9265001 | Specimen processing (procedure) | SNOMED Clinical Terms | | | 2‑L | 430854000 | Touch preparation of specimen (procedure) | SNOMED Clinical Terms | | | 2‑L | 448938001 | Preparation of smear (procedure) | SNOMED Clinical Terms | | | 2‑L | 77896007 | Cytopathology procedure, cell block and smear preparation (procedure) | SNOMED Clinical Terms | | | 2‑L | 4064007 | Specimen aliquoting (procedure) | SNOMED Clinical Terms | | | 2‑L | 8378006 | Trimming (procedure) | SNOMED Clinical Terms | | | 2‑L | 73373003 | Specimen centrifugation (procedure) | SNOMED Clinical Terms | | | 2‑L | 27872000 | Specimen freezing (procedure) | SNOMED Clinical Terms | | | 2‑L | 104166004 | Nucleic acid molecular isolation or extraction method (procedure) | SNOMED Clinical Terms | | | 2‑S | 13283003 | Tissue processing technique (procedure) | SNOMED Clinical Terms | | | 3‑L | 27204007 | Tissue frozen section technique, complete (procedure) | SNOMED Clinical Terms | | | 3‑L | 40923002 | Tissue processing technique, routine, embed, cut and stain, per surgical specimen (procedure) | SNOMED Clinical Terms | | | 4‑L | 434472006 | Sectioning of tissue block (procedure) | SNOMED Clinical Terms | | | 4‑L | 434475008 | Step sectioning of tissue block (procedure) | SNOMED Clinical Terms | | | 4‑L | 434474007 | Surface recutting of tissue block (procedure) | SNOMED Clinical Terms | | | 4‑L | 434479002 | Core sampling of tissue block (procedure) | SNOMED Clinical Terms | | | 4‑L | 433454009 | Microdissection of tissue specimen using laser (procedure) | SNOMED Clinical Terms | | | 4‑L | 702941008 | Paraffin embedding (qualifier value) | SNOMED Clinical Terms | | | 2‑S | 127790008 | Staining method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406792001 | Acid phosphatase stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406901007 | Neutrophil alkaline phosphatase stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406902000 | New fuchsin stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406903005 | Nile blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406904004 | Nitrazine yellow stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117229004 | Nonspecific esterase stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406905003 | Nuclear fast red stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406906002 | Orange G stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406907006 | Orange II stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406908001 | Page blue 83 stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406909009 | Page blue G-90 stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406910004 | Patent blue V sodium salt stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406911000 | Permethrin stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406912007 | Phloxin B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406913002 | Ponceau 3R stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406914008 | Ponceau S stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406915009 | Ponceau xylidine stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406916005 | Pontamine sky blue 5BX stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406900008 | Naphthol yellow S stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406899003 | Naphthol green B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406898006 | Naphthalene black 12B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117306005 | Lawson-Van Gieson stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406875003 | Leishman stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406876002 | Light green SF stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406877006 | Lissamine fast red B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406878001 | Lissamine fast yellow stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406880007 | Lissamine rhodamine stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 398507009 | Malachite green stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117218003 | Mallory bleach stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406890004 | Martius yellow stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406891000 | Meldola blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406892007 | Metanil yellow stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406893002 | Methyl blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406894008 | Methyl orange stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406895009 | Methyl red stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406896005 | Methylene blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406897001 | Methylene violet stain (Bernthsen) method (procedure) | SNOMED Clinical Terms | | | 3‑L | 37926009 | Microbial stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406917001 | Pontamine sky blue 6BX stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406918006 | Procion brilliant blue MRS stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117326009 | Quinacrine fluorescent stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406936006 | Sudan blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406937002 | Sunset yellow FCF stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117031001 | Supravital stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406938007 | Tartrazine stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406939004 | Thioflavine T stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406940002 | Thionine stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406941003 | Titan yellow stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406942005 | Tropaeolin O stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406943000 | Tropaeolin OO stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406944006 | Trypan blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406945007 | Vital new red stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 104249006 | Vital stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406946008 | Water soluble aniline blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406948009 | Water soluble anthracene brown stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406947004 | Water soluble nigrosine stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406949001 | Waxoline blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406950001 | Xylene cyanol FF stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406934009 | Sudan black stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406935005 | Sudan black B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117030000 | Sudan IV stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406919003 | Romanowsky stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406920009 | Rose bengal stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406921008 | Rosolic acid sodium salt stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406922001 | Saffron stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117330007 | Schmorl stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117041003 | Silver stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406924000 | Sirius red F3B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406925004 | Solochrome azurine (BS) stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406926003 | Solochrome black 6B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406927007 | Solochrome cyanine R stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406928002 | Solochrome dark blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406929005 | Soluble berlin blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406930000 | Spirit soluble aniline blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406931001 | Spirit soluble eosin stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406932008 | Spore stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406933003 | Sudan II stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117029005 | Sudan III stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406874004 | Lacmoid stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406873005 | Kenacid blue R stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406818007 | Bismark brown Y stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406819004 | Blue shade eosin stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406820005 | Brazilin stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406821009 | Brilliant cresyl blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406822002 | Brilliant crocein stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406823007 | Brilliant orange stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406824001 | Brilliant yellow stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 77281003 | Calcofluor white stain (procedure) | SNOMED Clinical Terms | | | 3‑L | 406825000 | Carminic acid stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406826004 | Carmoisine A stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406827008 | Celestine blue B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406828003 | Chloroacetate esterase stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406830001 | Chromotrope 2R stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406831002 | Chrysoidine R stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406832009 | Chrysoidine Y stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406833004 | Cochineal stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117055006 | Congo red stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406817002 | Bismark brown R stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406816006 | Biebrich scarlet stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406815005 | Beta-glucuronidase stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406793006 | Albert's stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117036006 | Alcian blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406794000 | Alcohol soluble nigrosine stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406795004 | Alizarin blue S stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406796003 | Alizarin cyanine green stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406797007 | Alizarin red S stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406798002 | Alizarin yellow GG stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406799005 | Alizarin yellow R stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406800009 | Auramine stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406801008 | Azo black stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406802001 | Azocarmine G (GX) stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406803006 | Azophloxin stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406804000 | Azorubin S stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406811001 | Azure A stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406812008 | Azure B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406813003 | Azure C stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406814009 | Benzo fast scarlet stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406835006 | Crystal ponceau stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406836007 | Curcumin stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117298004 | Cytopathology staining method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406857004 | Flagellar stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406858009 | Fluorescent stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406863008 | Fuchsin acid stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 117047004 | Fuchsin basic stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 20543007 | Fungus stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406864002 | Gallocyanine stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 422329009 | Hall's bilirubin stain (procedure) | SNOMED Clinical Terms | | | 3‑L | 406865001 | Hematein stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 108256005 | Hematology staining procedure (procedure) | SNOMED Clinical Terms | | | 3‑L | 406867009 | Immunofluorescent stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406868004 | Indigo carmine stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406869007 | Indophenol from naphthol stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406870008 | Insoluble berlin blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406871007 | Janus green B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406872000 | Jenner-Giemsa stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406856008 | Field's stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406855007 | Feulgen reaction stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406854006 | Fat red 7B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406837003 | Diamond black stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406838008 | Durazol red stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406839000 | Erie garnet stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406840003 | Eriochrome blue black SE stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406841004 | Erythrosin B stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406842006 | Erythrosin Y stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406843001 | Evans blue stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406844007 | Fast blue B salt stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406845008 | Fast blue BB salt stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406846009 | Fast blue RR salt stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406847000 | Fast garnet GBC salt stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406848005 | Fast green FCF stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406849002 | Fast red B salt stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406850002 | Fast red ITR stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406851003 | Fast red TR salt stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406852005 | Fast sulfon black F stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406853000 | Fast violet B salt stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 406979008 | Ziehl-Neelsen stain method (procedure) | SNOMED Clinical Terms | | | 3‑S | 104210008 | Hematoxylin and eosin stain method (procedure) | SNOMED Clinical Terms | | | 4‑L | 117239005 | Harris regressive hematoxylin and eosin stain method (procedure) | SNOMED Clinical Terms | | | 4‑L | 117240007 | Mayers progressive hematoxylin and eosin stain method (procedure) | SNOMED Clinical Terms | | | 3‑L | 80246006 | Special stain, blood or bone marrow, explain by report (procedure) | SNOMED Clinical Terms | | | 3‑L | 117617002 | Immunohistochemistry procedure (procedure) | SNOMED Clinical Terms | | | 3‑L | 384715000 | Nucleic acid hybridization procedure (procedure) | SNOMED Clinical Terms | |
|
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC stage 1.3.6.1.4.1.19376.1.3.11.18
| Id | 1.3.6.1.4.1.19376.1.3.11.18 | Effective Date | valid from 2015‑06‑23 16:43:02 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICCstage | Display Name | UICC Stage (7ed) |
|---|
| Description |  UICC Stages<br clear="none"/> |
|---|
| Source Code System | 2.16.840.1.113883.15.6 - TNM Edition7 UICC |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | okk | stage X | TNM Edition7 UICC | TX, N0, M0 | | 0‑S | 0 | stage 0 | TNM Edition7 UICC | Tis N0 M0 | | 1‑L | 0a | stage 0a | TNM Edition7 UICC | in C67 only | | 1‑L | 0is | stage 0is | TNM Edition7 UICC | in C67 only | | 0‑S | I | stage I | TNM Edition7 UICC | organ dependent | | 2‑L | IA1 | stage IA1 | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 2‑L | IA2 | stage IA2 | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 1‑S | IB | stage IB | TNM Edition7 UICC | organ dependent | | 2‑L | IB1 | stage IB1 | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 2‑L | IB2 | stage IB2 | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 1‑L | IC | stage IC | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 1‑L | IS | stage IS | TNM Edition7 UICC | in C62 only | | 0‑S | II | stage II | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 2‑L | IIA | stage IIA | TNM Edition7 UICC | organ dependent<br clear="none"/>
<br clear="none"/> | | 2‑L | IIA1 | stage IIA1 | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 2‑L | IIA2 | stage IIA2 | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 1‑L | IIB | stage IIB | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 1‑L | IIC | stage IIC | TNM Edition7 UICC | organ dependent<br clear="none"/>
<br clear="none"/> | | 0‑S | III | stage III | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 1‑L | IIIA | stage IIIA | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 1‑L | IIIB | stage IIIB | TNM Edition7 UICC | organ dependent<br clear="none"/>
<br clear="none"/> | | 1‑L | IIIC | stage IIIC | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 0‑S | IV | stage IV | TNM Edition7 UICC | each T, each N, M1 | | 1‑L | IVA | stage IVA | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 1‑L | IVB | stage IVB | TNM Edition7 UICC | organ dependent<br clear="none"/> | | 1‑L | IVC | stage IVC | TNM Edition7 UICC | organ dependent<br clear="none"/> |
|
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC T category 1.3.6.1.4.1.19376.1.3.11.15
| Id | 1.3.6.1.4.1.19376.1.3.11.15 | Effective Date | valid from 2015‑11‑11 14:05:36 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-t-value-7ed | Display Name | UICC T category (7ed) |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.15.6 - TNM Edition7 UICC 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | Ta | Ta | TNM Edition7 UICC | | 0‑L | Tis | Tis | TNM Edition7 UICC | | 1‑L | Tis(DCIS) | Tis(DCIS) | TNM Edition7 UICC | | 1‑L | Tis(LCIS) | Tis(LCIS) | TNM Edition7 UICC | | 1‑L | Tis(Paget) | Tis(Paget) | TNM Edition7 UICC | | 1‑L | Tis(pu) | Tis(pu) | TNM Edition7 UICC | | 1‑L | Tis(pd) | Tis(pd) | TNM Edition7 UICC | | 0‑L | T0 | T0 | TNM Edition7 UICC | | 0‑L | T1 | T1 | TNM Edition7 UICC | | 1‑L | T1mi | T1mi | TNM Edition7 UICC | | 1‑L | T1a | T1a | TNM Edition7 UICC | | 2‑L | T1a1 | T1a1 | TNM Edition7 UICC | | 2‑L | T1a2 | T1a2 | TNM Edition7 UICC | | 1‑L | T1b | T1b | TNM Edition7 UICC | | 2‑L | T1b1 | T1b1 | TNM Edition7 UICC | | 2‑L | T1b2 | T1b2 | TNM Edition7 UICC | | 1‑L | T1c | T1c | TNM Edition7 UICC | | 1‑L | T1d | T1d | TNM Edition7 UICC | | 0‑L | T2 | T2 | TNM Edition7 UICC | | 1‑L | T2a | T2a | TNM Edition7 UICC | | 2‑L | T2a1 | T2a1 | TNM Edition7 UICC | | 2‑L | T2a2 | T2a2 | TNM Edition7 UICC | | 1‑L | T2b | T2b | TNM Edition7 UICC | | 1‑L | T2c | T2c | TNM Edition7 UICC | | 1‑L | T2d | T2d | TNM Edition7 UICC | | 0‑L | T3 | T3 | TNM Edition7 UICC | | 1‑L | T3a | T3a | TNM Edition7 UICC | | 1‑L | T3b | T3b | TNM Edition7 UICC | | 1‑L | T3c | T3c | TNM Edition7 UICC | | 1‑L | T3d | T3d | TNM Edition7 UICC | | 0‑L | T4 | T4 | TNM Edition7 UICC | | 1‑L | T4a | T4a | TNM Edition7 UICC | | 1‑L | T4b | T4b | TNM Edition7 UICC | | 1‑L | T4c | T4c | TNM Edition7 UICC | | 1‑L | T4d | T4d | TNM Edition7 UICC | | 1‑L | T4e | T4e | TNM Edition7 UICC | | 0‑L | Tx | TX | TNM Edition7 UICC |
| | 0‑L | ASKU | Asked, but unknown | Null Flavor |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC T category (SCT) 1.3.6.1.4.1.19376.1.3.11.12
| Id | 1.3.6.1.4.1.19376.1.3.11.12 | Effective Date | valid from 2014‑05‑13 15:52:43 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-t-value5 | Display Name | UICC T category (SCT) |
|---|
| Description | T-Value from UICC classification |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.6.96 - SNOMED Clinical Terms 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | 261663004 | Tumor stage Ta (tumor staging) | SNOMED Clinical Terms | | 0‑S | 44401000 | Tis category (finding) | SNOMED Clinical Terms | | 1‑L | 313145008 | Tumor stage Tis pu (finding) | SNOMED Clinical Terms | | 1‑L | 313146009 | Tumor stage Tis pd (finding) | SNOMED Clinical Terms | | 0‑L | 58790005 | T0 category (finding) | SNOMED Clinical Terms | | 0‑S | 23351008 | T1 category (finding) | SNOMED Clinical Terms | | 1‑L | 313108002 | Tumor stage T1mic (finding) | SNOMED Clinical Terms | | 1‑L | 261646003 | Tumor stage T1a (finding) | SNOMED Clinical Terms | | 2‑L | 261647007 | Tumor stage T1a1 (finding) | SNOMED Clinical Terms | | 2‑L | 261648002 | Tumor stage T1a2 (finding) | SNOMED Clinical Terms | | 1‑L | 261649005 | Tumor stage T1b (finding) | SNOMED Clinical Terms | | 2‑L | 313110000 | Tumor stage T1b1 (finding) | SNOMED Clinical Terms | | 2‑L | 313111001 | Tumor stage T1b2 (finding) | SNOMED Clinical Terms | | 1‑L | 261650005 | Tumor stage T1c (finding) | SNOMED Clinical Terms | | 0‑S | 67673008 | T2 category (finding) | SNOMED Clinical Terms | | 1‑L | 261651009 | Tumor stage T2a (finding) | SNOMED Clinical Terms | | 1‑L | 261652002 | Tumor stage T2b (finding) | SNOMED Clinical Terms | | 1‑L | 261653007 | Tumor stage T2c (finding) | SNOMED Clinical Terms | | 0‑S | 14410001 | T3 category (finding) | SNOMED Clinical Terms | | 1‑L | 261654001 | Tumor stage T3a (finding) | SNOMED Clinical Terms | | 1‑L | 261655000 | Tumor stage T3b (finding) | SNOMED Clinical Terms | | 2‑L | 261656004 | Tumor stage T3bi (finding) | SNOMED Clinical Terms | | 2‑L | 261657008 | Tumor stage T3bii (finding) | SNOMED Clinical Terms | | 1‑L | 261658003 | Tumor stage T3c (finding) | SNOMED Clinical Terms | | 0‑S | 65565005 | T4 category (finding) | SNOMED Clinical Terms | | 1‑L | 261659006 | Tumor stage T4a (finding) | SNOMED Clinical Terms | | 1‑L | 261660001 | Tumor stage T4b (finding) | SNOMED Clinical Terms | | 1‑L | 261661002 | Tumor stage T4c (finding) | SNOMED Clinical Terms | | 1‑L | 261662009 | Tumor stage T4d (finding) | SNOMED Clinical Terms | | 0‑L | 67101007 | TX category (finding) | SNOMED Clinical Terms |
| | 0‑L | ASKU | Asked but unknown | Null Flavor |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC N category 1.3.6.1.4.1.19376.1.3.11.16
| Id | 1.3.6.1.4.1.19376.1.3.11.16 | Effective Date | valid from 2015‑11‑11 14:45:19 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC_n_value | Display Name | UICC N category (7ed) |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.15.6 - TNM Edition7 UICC 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | N0 | N0 | TNM Edition7 UICC | | 0‑L | N1 | N1 | TNM Edition7 UICC | | 1‑L | N1mi | N1mi | TNM Edition7 UICC | | 1‑L | N1a | N1a | TNM Edition7 UICC | | 1‑L | N1b | N1b | TNM Edition7 UICC | | 1‑L | N1c | N1c | TNM Edition7 UICC | | 0‑L | N2 | N2 | TNM Edition7 UICC | | 1‑L | N2mi | N2mi | TNM Edition7 UICC | | 1‑L | N2a | N2a | TNM Edition7 UICC | | 1‑L | N2b | N2b | TNM Edition7 UICC | | 1‑L | N2c | N2c | TNM Edition7 UICC | | 0‑L | N3 | N3 | TNM Edition7 UICC | | 1‑L | N3mi | N3mi | TNM Edition7 UICC | | 1‑L | N3a | N3a | TNM Edition7 UICC | | 1‑L | N3b | N3b | TNM Edition7 UICC | | 1‑L | N3c | N3c | TNM Edition7 UICC | | 0‑L | NX | Nx | TNM Edition7 UICC |
| | 0‑L | ASKU | Asked but unknown | Null Flavor |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC N category (SCT) 1.3.6.1.4.1.19376.1.3.11.13
| Id | 1.3.6.1.4.1.19376.1.3.11.13 | Effective Date | valid from 2014‑10‑27 14:47:35 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC_N_values | Display Name | UICC N category (SCT) |
|---|
| Description | N-Value from UICC classification |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.6.96 - SNOMED Clinical Terms 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | 62455006 | N0 category (finding) | SNOMED Clinical Terms | | 0‑L | 53623008 | N1 category (finding) | SNOMED Clinical Terms | | 1‑L | 277672002 | Node stage N1a (finding) | SNOMED Clinical Terms | | 1‑L | 277674001 | Node stage N1b (finding) | SNOMED Clinical Terms | | 2‑L | 277772008 | Node stage N1bi (finding) | SNOMED Clinical Terms | | 2‑L | 277776006 | Node stage N1bii (finding) | SNOMED Clinical Terms | | 2‑L | 277777002 | Node stage N1biii (finding) | SNOMED Clinical Terms | | 2‑L | 277778007 | Node stage N1biv (finding) | SNOMED Clinical Terms | | 1‑L | 369996002 | N1c: >7 nodes involved (finding) | SNOMED Clinical Terms | | 0‑L | 46059003 | N2 category (finding) | SNOMED Clinical Terms | | 1‑L | 261967001 | Node stage N2a (finding) | SNOMED Clinical Terms | | 1‑L | 261968006 | Node stage N2b (finding) | SNOMED Clinical Terms | | 1‑L | 261969003 | Node stage N2c (finding) | SNOMED Clinical Terms | | 0‑L | 5856006 | N3 category (finding) | SNOMED Clinical Terms | | 1‑L | 370012005 | N3a: > 6 cm in dimension (finding) | SNOMED Clinical Terms | | 1‑L | 370013000 | N3b: extension to supraclavicular fossa (finding) | SNOMED Clinical Terms | | 0‑L | 79420006 | NX category (finding) | SNOMED Clinical Terms |
| | 0‑L | ASKU | Asked but unknown | Null Flavor |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC M category 1.3.6.1.4.1.19376.1.3.11.17
| Id | 1.3.6.1.4.1.19376.1.3.11.17 | Effective Date | valid from 2015‑11‑11 15:53:15 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-m-values | Display Name | UICC M category (7ed) |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.15.6 - TNM Edition7 UICC 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | M0 | M0 | TNM Edition7 UICC | | 0‑L | M1 | M1 | TNM Edition7 UICC | | 1‑L | M1mi | M1(mi) | TNM Edition7 UICC | | 1‑L | M1a | M1a | TNM Edition7 UICC | | 1‑L | M1b | M1b | TNM Edition7 UICC | | 1‑L | M1c | M1c | TNM Edition7 UICC | | 1‑L | M1d | M1d | TNM Edition7 UICC | | 1‑L | M1e | M1e | TNM Edition7 UICC | | 1‑L | M1cy | M1(cy) | TNM Edition7 UICC | | 0‑L | MX | MX | TNM Edition7 UICC |
| | 0‑L | ASKU | Asked but unknown | Null Flavor |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC M category (SCT) 1.3.6.1.4.1.19376.1.3.11.14
| Id | 1.3.6.1.4.1.19376.1.3.11.14 | Effective Date | valid from 2014‑05‑13 16:11:15 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-m-value | Display Name | UICC M category (SCT) |
|---|
| Description | M-Value from UICC classification |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.6.96 - SNOMED Clinical Terms 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | 30893008 | M0 category (finding) | SNOMED Clinical Terms | | 0‑L | 55440008 | M1 category (finding) | SNOMED Clinical Terms | | 1‑L | 261927002 | Metastasis stage M1a (finding) | SNOMED Clinical Terms | | 1‑L | 261928007 | Metastasis stage M1b (finding) | SNOMED Clinical Terms | | 1‑L | 261929004 | Metastasis stage M1c (finding) | SNOMED Clinical Terms | | 0‑L | 27167007 | MX category (finding) | SNOMED Clinical Terms |
| | 0‑L | ASKU | Asked but unknown | Null Flavor |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC C-Factor 1.3.6.1.4.1.19376.1.3.11.19
| Id | 1.3.6.1.4.1.19376.1.3.11.19 | Effective Date | valid from 2015‑11‑13 13:56:23 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | uicc-c-factor-tnm | Display Name | UICC C-Factor |
|---|
| Description | Qualifier for any TNM category coding the certainty of classification by the methods used
|
|---|
| Source Code System | 2.16.840.1.113883.15.6 - TNM Edition7 UICC |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | C1 | C1 | TNM Edition7 UICC | | 0‑L | C2 | C2 | TNM Edition7 UICC | | 0‑L | C3 | C3 | TNM Edition7 UICC | | 0‑L | C4 | C4 | TNM Edition7 UICC | | 0‑L | C5 | C5 | TNM Edition7 UICC |
|
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC C-Factor (SCT) 1.3.6.1.4.1.19376.1.3.11.20
| Id | 1.3.6.1.4.1.19376.1.3.11.20 | Effective Date | valid from 2015‑06‑22 15:47:55 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | uicc-c-factor | Display Name | UICC C-Factor (SCT) |
|---|
| Description | Qualifier for any TNM category coding the certainty of classification by the methods used |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
| Source Code System | 2.16.840.1.113883.6.96 - SNOMED Clinical Terms |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | 84068000 | C1 - TNM certainty factor | SNOMED Clinical Terms | | 0‑L | 76321005 | C2 - TNM certainty factor | SNOMED Clinical Terms | | 0‑L | 44756004 | C3 - TNM certainty factor | SNOMED Clinical Terms | | 0‑L | 75800005 | C4 - TNM certainty factor | SNOMED Clinical Terms | | 0‑L | 59397002 | C5 - TNM certainty factor | SNOMED Clinical Terms |
|
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Residual tumor (R) classification 1.3.6.1.4.1.19376.1.3.11.21
| Id | 1.3.6.1.4.1.19376.1.3.11.21 | Effective Date | valid from 2015‑06‑25 11:23:51 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-R-status | Display Name | UICC Residual tumor (R) classification |
|---|
| Description | Value set for Residual tumor state with values for extended R-Klassifikation (TNM Suppl. 4th ed.) |
|---|
| Copyright | This artefact includes content from SNOMED Clinical Terms® (SNOMED CT®) which is copyright of the International Health Terminology Standards Development Organisation (IHTSDO). Implementers of these artefacts must have the appropriate SNOMED CT Affiliate license - for more information contact http://www.snomed.org/snomed-ct/getsnomed-ct or info@snomed.org. |
|---|
| 5 Source Code Systems | 2.16.840.1.113883.6.96 - SNOMED Clinical Terms 2.16.840.1.113883.15.16 - TNM Edition8 UICC 2.16.840.1.113883.15.6 - TNM Edition7 UICC 1.2.276.0.76.3.1.131.1.5.120 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | 258254000 | Residual tumor stage R0 (finding) | SNOMED Clinical Terms | | | 1‑L | 415675004 | Surgical circumferential margin is closest uninvolved margin to malignant neoplasm (finding) | SNOMED Clinical Terms | No residual tumor: R0 > 1mm CRM negative | | 0‑L | 278271003 | Residual tumor stage R1 (finding) | SNOMED Clinical Terms | | | 1‑L | 384620009 | Surgical circumferential margin involved by malignant neoplasm (tumor present 0-1 mm from circumferential resection margin) (finding) | SNOMED Clinical Terms | | | 0‑L | 278272005 | Residual tumor stage R2 (finding) | SNOMED Clinical Terms | | | 0‑L | 258253006 | Residual tumor stage RX (finding) | SNOMED Clinical Terms | | | 0‑L | RX | RX | TNM Edition8 UICC | | | 0‑L | R0>1mm | R0 > 1mm | TNM Edition7 UICC | | | 0‑L | R0<1mm | R0 < 1mm | TNM Edition7 UICC | | | 0‑L | R1 | R1 | TNM Edition8 UICC | | | 1‑L | R1-dir | R1-dir | TNM Edition7 UICC | | | 1‑L | R1(is) | R1(is) | 1.2.276.0.76.3.1.131.1.5.120 | | | 1‑L | R1(cy) | R1(cy) | 1.2.276.0.76.3.1.131.1.5.120 | | | 0‑L | R2 | R2 | TNM Edition8 UICC | | | 1‑L | R2a | R2a | TNM Edition7 UICC | | | 1‑L | R2b | R2b | TNM Edition7 UICC | | | 1‑L | R2c | R2c | TNM Edition7 UICC | | | 0‑L | CRM+ | CRM positive | TNM Edition7 UICC | | | 0‑L | CRM- | CRM negative | TNM Edition7 UICC | |
| | 0‑L | ASKU | Asked but unknown | Null Flavor | |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC clinical/pathological 1.3.6.1.4.1.19376.1.3.11.22
| Id | 1.3.6.1.4.1.19376.1.3.11.22 | Effective Date | valid from 2015‑11‑04 15:52:34 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-clinical-pathological | Display Name | UICC clinical/pathological |
|---|
| Description | Qualifiers for each TNM category classifying the observation method and the time frame of observation in relation to treatment |
|---|
| 3 Source Code Systems | 2.16.840.1.113883.15.16 - TNM Edition8 UICC 1.2.276.0.76.11.9 - hl7de-valueset-9 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | p | p | TNM Edition8 UICC | The pathological assessment of the primary tumor entails a resection of the primary tumor or a biopsy adequate to evaluate the highest T category. The pathological assessment of the regional lymph nodes entails a removal of lymph nodes adequate to validate the absence of regional lymph node metastasis or sufficient to evaluate the highest pN category. The pathological assessment of distant metastasis entails microscopic examination. | | 0‑L | c | c | TNM Edition8 UICC | The clinical classification is based on evidence acquired before treatment | | 1‑L | u | u | hl7de-valueset-9 | The clinical classification is based on ultrasound evidence acquired before treatment | | 1‑L | ct | ct | hl7de-valueset-9 | The clinical classification is based on CT imaging evidence acquired before treatment | | 1‑L | mr | mr | hl7de-valueset-9 | The clinical classification is based on magnetic resonance imaging evidence acquired before treatment |
| | 0‑L | ASKU | Asked but unknown | Null Flavor | |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Venous Invasion 1.3.6.1.4.1.19376.1.3.11.23
| Id | 1.3.6.1.4.1.19376.1.3.11.23 | Effective Date | valid from 2015‑11‑04 16:17:55 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-vene-invasion | Display Name | UICC Venous Invasion |
|---|
| Description | Observation for tumor spread coding the degree of venous invasion
|
|---|
| 2 Source Code Systems | 2.16.840.1.113883.15.16 - TNM Edition8 UICC 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | V0 | V0 | TNM Edition8 UICC | | 0‑L | V1 | V1 | TNM Edition8 UICC | | 0‑L | V2 | V2 | TNM Edition8 UICC | | 0‑L | VX | VX | TNM Edition8 UICC |
| | 0‑L | ASKU | Asked but unknown | Null Flavor |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Lymphatic Invasion 1.3.6.1.4.1.19376.1.3.11.24
| Id | 1.3.6.1.4.1.19376.1.3.11.24 | Effective Date | valid from 2015‑11‑04 16:19:20 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-lymphatic-invasion | Display Name | UICC Lymphatic Invasion |
|---|
| Description | Observation for tumor spread coding the degree of lymphatic invasion |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.15.16 - TNM Edition8 UICC 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | L0 | L0 | TNM Edition8 UICC | | 0‑L | L1 | L1 | TNM Edition8 UICC | | 0‑L | LX | LX | TNM Edition8 UICC |
| | 0‑L | ASKU | Asked but unknown | Null Flavor |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Perineurial Invasion 1.3.6.1.4.1.19376.1.3.11.25
| Id | 1.3.6.1.4.1.19376.1.3.11.25 | Effective Date | valid from 2015‑11‑04 16:20:42 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-perineural-invasion | Display Name | UICC Perineural Invasion |
|---|
| Description |
Observation for tumor spread coding the degree of perineural (lymphatic nerve sheet) invasion
|
|---|
| 2 Source Code Systems | 2.16.840.1.113883.15.16 - TNM Edition8 UICC 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | Pn0 | Pn0 | TNM Edition8 UICC | no perineural invasion
| | 0‑L | Pn1 | Pn1 | TNM Edition8 UICC | Perineural invasion
| | 0‑L | PnX | PnX | TNM Edition8 UICC | unknown
|
| | 0‑L | ASKU | Asked but unknown | Null Flavor | |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Mucosa 1.3.6.1.4.1.19376.1.3.11.26
| Id | 1.3.6.1.4.1.19376.1.3.11.26 | Effective Date | valid from 2015‑11‑04 16:22:04 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-mucosa | Display Name | UICC Mucosa |
|---|
| Source Code System | 1.2.276.0.76.3.1.131.1.5.1 |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | m1 | m1 | 1.2.276.0.76.3.1.131.1.5.1 | restricted to mucosa, 1st third
| | 0‑L | m2 | m2 | 1.2.276.0.76.3.1.131.1.5.1 | restricted to mucosa, 2nd third
| | 0‑L | m3 | m3 | 1.2.276.0.76.3.1.131.1.5.1 | restricted to mucosa, 3rd third
|
|
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Submucosa 1.3.6.1.4.1.19376.1.3.11.27
| Id | 1.3.6.1.4.1.19376.1.3.11.27 | Effective Date | valid from 2015‑11‑04 16:23:24 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-submucosa | Display Name | UICC Submucosa |
|---|
| Source Code System | 1.2.276.0.76.3.1.131.1.5.1 |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | sm1 | sm1 | 1.2.276.0.76.3.1.131.1.5.1 | restricted to submucosa, 1st third
| | 0‑L | sm2 | sm2 | 1.2.276.0.76.3.1.131.1.5.1 | restricted to submucosa, 2nd third
| | 0‑L | sm3 | sm3 | 1.2.276.0.76.3.1.131.1.5.1 | restricted to submucosa, 3rd third
|
|
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Localization of distant metastases 1.3.6.1.4.1.19376.1.3.11.28
| Id | 1.3.6.1.4.1.19376.1.3.11.28 | Effective Date | valid from 2015‑11‑04 16:26:53 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICC-distant-metastasis-localization | Display Name | UICC Localization of distant metastases |
|---|
| Description | Qualifier for M category coding the localization of distant metastasis in case of M1 or M2 |
|---|
| Source Code System | 2.16.840.1.113883.15.16 - TNM Edition8 UICC |
|---|
| Level/ Type | Code | Display Name | Code System |
|---|
| 0‑L | PUL | PUL | TNM Edition8 UICC | | 0‑L | OSS | OSS | TNM Edition8 UICC | | 0‑L | HEP | HEP | TNM Edition8 UICC | | 0‑L | BRA | BRA | TNM Edition8 UICC | | 0‑L | LYM | LYM | TNM Edition8 UICC | | 0‑L | OTH | OTH | TNM Edition8 UICC | | 0‑L | MAR | MAR | TNM Edition8 UICC | | 0‑L | PLE | PLE | TNM Edition8 UICC | | 0‑L | PER | PER | TNM Edition8 UICC | | 0‑L | ADR | ADR | TNM Edition8 UICC | | 0‑L | SKI | SKI | TNM Edition8 UICC |
|
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Grade 3 tiered 1.3.6.1.4.1.19376.1.3.11.29
| Id | 1.3.6.1.4.1.19376.1.3.11.29 | Effective Date | valid from 2015‑11‑13 19:36:21 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICCgrade | Display Name | UICC Grade 3 tiered |
|---|
| Description | Coding of the grade of differentiation (malignancy) of tumors, coded by a four-, three-, or two-tiered grading system, often using the score of a special grading system for certain tumor types |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.15.16 - TNM Edition8 UICC 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | 1 | G1 | TNM Edition8 UICC | grade 1, well (highly) differentiated | | 0‑L | 2 | G2 | TNM Edition8 UICC | grade 2, moderately differentiated | | 0‑L | 3 | G3 | TNM Edition8 UICC | grade 3, poorly differentiated | | 0‑L | X | GX | TNM Edition8 UICC | cannot be assessed |
| | 0‑L | ASKU | Asked but unknown | Null Flavor | |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Grade 2 tiered 1.3.6.1.4.1.19376.1.3.11.30
| Id | 1.3.6.1.4.1.19376.1.3.11.30 | Effective Date | valid from 2015‑11‑13 19:43:09 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICCgrade-2 | Display Name | UICC Grade 2 tiered |
|---|
| Description | Coding of the grade of differentiation (malignancy) of tumors, coded by a two-tiered grading system, sometimes using the score of a special grading system for certain tumor types |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.15.16 - TNM Edition8 UICC 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | L | lG | TNM Edition8 UICC | low grade, combining grade 1 and 2 (except urothelial tumors: only grade 1) | | 0‑L | H | hG | TNM Edition8 UICC | low grade, combining grade 3 and 4 (except urothelial tumors: grade 2 through 4) | | 0‑L | X | X | TNM Edition8 UICC | cannot be assessed |
| | 0‑L | ASKU | Asked but unknown | Null Flavor | |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Grade 4 tiered 1.3.6.1.4.1.19376.1.3.11.31
| Id | 1.3.6.1.4.1.19376.1.3.11.31 | Effective Date | valid from 2015‑11‑13 19:46:53 |
|---|
| Status |  Draft Draft | Version Label | |
|---|
| Name | UICCgrade-4 | Display Name | UICC Grade 4 tiered |
|---|
| Description | Coding of the grade of differentiation (malignancy) of tumors, coded by a four-tiered grading system, sometimes using the score of a special grading system for certain tumor types. |
|---|
| 3 Source Code Systems | 2.16.840.1.113883.15.16 - TNM Edition8 UICC 1.2.276.0.76.5.336 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | 1 | G1 | TNM Edition8 UICC | well (highly) differentiated | | 0‑L | 2 | G2 | TNM Edition8 UICC | moderately differentiated | | 0‑L | 3 | G3 | TNM Edition8 UICC | poorly differentiated | | 0‑L | 4 | G4 | TNM Edition8 UICC | undifferentiated resp. anaplastic | | 0‑L | X | GX | TNM Edition8 UICC | cannot be assessed | | 0‑L | 0 | 0 | 1.2.276.0.76.5.336 | Malignes Melanom der Konjunktiva | | 0‑L | X | X | 1.2.276.0.76.5.336 | nicht bestimmbar | | 0‑L | L | lG | 1.2.276.0.76.5.336 | Low grade (G1 oder G2) | | 0‑L | M | mG | 1.2.276.0.76.5.336 | intermediate (G2 oder G3) | | 0‑L | H | hG | 1.2.276.0.76.5.336 | high grade (G3 oder G4) | | 0‑L | B | B | 1.2.276.0.76.5.336 | Borderline-Malignität | | 0‑L | U | U | 1.2.276.0.76.5.336 | unbekannt | | 0‑L | T | T | 1.2.276.0.76.5.336 | trifft nicht zu |
| | 0‑L | ASKU | Asked but unknown | Null Flavor | |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
UICC/AJCC Tumor Serum Markers 1.3.6.1.4.1.19376.1.3.11.32
| Beschreibung |
|---|
 Observation of serum levels of tumor markers coded for germ cell tumors Observation of serum levels of tumor markers coded for germ cell tumors | | Value Set Name | Value Set Id | Version / Eingangsdatum | Status |
|---|
| UICCSerumTumorMarkers | 2.16.840.1.113883.2.6.60.6.11.21 | 2015‑11‑08 18:26:39 | Entwurf | Ein gültiger Code aus der Codesystem:| Codesystem Name | Codesystem Id | Codesystem Version | | TNM Edition7 UICC | 2.16.840.1.113883.15.6 | |
| | Or one of the following: | Quell-Codesystem:- 2.16.840.1.113883.15.6 UICC 7. Auflage
- 2.16.840.1.113883.6.96 SNOMED Clinical Terms
| | Level/ Typ | Code | Anzeigename | Codesystem | Beschreibung | | 0-L | S0 | S0 | UICC 7. Auflage | | | 0-L | S1 | S1 | UICC 7. Auflage | | | 0-L | S2 | S2 | UICC 7. Auflage | | | 0-L | S3 | S3 | SNOMED Clinical Terms | | | 0-L | SX | SX | UICC 7. Auflage | |
| | Legende: Typ L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors werden im @nullFlavor Attribut statt in @code angegeben. |
|
ICD-O-3 Morphology 1.3.6.1.4.1.19376.1.3.11.33
| Id | 1.3.6.1.4.1.19376.1.3.11.33 | Effective Date | valid from 2015‑11‑13 14:08:46 |
|---|
| Status |  Draft Draft | Version Label | 1st rev. (2013) |
|---|
| Name | icd-o-3-m | Display Name | ICD-O-3 Morphology |
|---|
| Description | International classification of diseases / oncology, morphological part for typing of benign and malignant tumors. The morphology axis provides six-digit codes ranging from 8000/0 to 9989/3. The first four digits indicate the specific histological term, i.e. morphology (8000 through 9992). <span style="text-align: justify;">In developing the previous editions and the present edition of ICD-O, a particular effort was made to use the nomenclature appearing in the World Health Organization </span>
<span style="text-align: justify;">International Histological Classification of Tumours</span> <span style="text-align: justify;">series (WHO “Blue Books”)</span>
<span style="text-align: justify;">7</span>
<span style="text-align: justify;">. This series covers all the principal sites of cancer and includes the morphology codes of ICD-O for each neoplasm. </span>All new histological classifications or modifications have been made by the WHO / IARC in so-called "Blue Books" by  2011 are listed on-line: http://codes.iarc.fr/changes.php.<br clear="none"/>The fifth digit after a slash (/) is the behavior code, which indicates whether a tumor is malignant, benign, in situ, or uncertain (whether benign or malignant). <br clear="none"/>A separate, 6th, one-digit code may also be given for histologic 4-tiered grading (differentiation) or for the cell type in lymphatic neoplasia.  <br clear="none"/>The fifth and the sixth digit are coded separately in value sets 1.3.6.1.4.1.19376.1.3.11.34 and 1.3.6.1.4.1.19376.1.3.11.35 |
|---|
A valid code from the code system:| Code System Name | Code System Id | Code System Version | | International Classification of Diseases for Oncology, version 3. | 2.16.840.1.113883.6.43.1 | |
|
| Or one of the following: |
| 2 Source Code Systems | 2.16.840.1.113883.6.43.1 - International Classification of Diseases for Oncology, version 3. 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | | Code System |
|---|
| | 0‑L | ASKU | Asked but unknown | Null Flavor |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
ICD-O-3 Behavior 1.3.6.1.4.1.19376.1.3.11.34
| Id | 1.3.6.1.4.1.19376.1.3.11.34 | Effective Date | valid from 2015‑11‑13 18:54:30 |
|---|
| Status |  Draft Draft | Version Label | 1st rev. (2013) |
|---|
| Name | icd-o-3-behavior | Display Name | ICD-O-3 Behavior |
|---|
| Description | Coding of the behavior of a tumor, coded by the first digit after slash in ICD-O-Morphology code |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.6.43.1 - International Classification of Diseases for Oncology, version 3. 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | 0 | /0 | International Classification of Diseases for Oncology, version 3. | benign | | 0‑L | 1 | /1 | International Classification of Diseases for Oncology, version 3. | borderline malignancy or uncertain malignant potential | | 0‑L | 2 | /2 | International Classification of Diseases for Oncology, version 3. | noninvasiv resp. carcinoma in situ | | 0‑L | 3 | /3 | International Classification of Diseases for Oncology, version 3. | invasive resp. malignant primary tumor | | 0‑L | 6 | /6 | International Classification of Diseases for Oncology, version 3. | metastasis resp. secondary tumor, not used in German cancer registries | | 0‑L | 9 | /9 | International Classification of Diseases for Oncology, version 3. | malignant, uncertain whether primary or secondary tumor, not used in German cancer registries |
| | 0‑L | ASKU | asked but unknown | Null Flavor | |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
ICD-O-3 Differentiation 1.3.6.1.4.1.19376.1.3.11.35
| Id | 1.3.6.1.4.1.19376.1.3.11.35 | Effective Date | valid from 2015‑11‑13 19:07:32 |
|---|
| Status |  Draft Draft | Version Label | 1st rev. (2013) |
|---|
| Name | icd-o-3-differentiation | Display Name | ICD-O-3 Differentiation |
|---|
| Description | Coding the cellular differentiation of malignant tumors, either the grade of malignancy (differentiation), or the cell line differentiation, coded by the second digit after the slash in ICD-O-3 Morphology axi |
|---|
| 2 Source Code Systems | 2.16.840.1.113883.6.43.1 - International Classification of Diseases for Oncology, version 3. 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | Display Name | Code System | Description |
|---|
| 0‑L | 1 | 1 | International Classification of Diseases for Oncology, version 3. | well (highly) differentiated | | 0‑L | 2 | 2 | International Classification of Diseases for Oncology, version 3. | moderately differentiated | | 0‑L | 3 | 3 | International Classification of Diseases for Oncology, version 3. | poorly differentiated | | 0‑L | 4 | 4 | International Classification of Diseases for Oncology, version 3. | undifferentiated resp. anaplastic | | 0‑L | 5 | 5 | International Classification of Diseases for Oncology, version 3. | T-cell differentiation in lymphomas and leukemias | | 0‑L | 6 | 6 | International Classification of Diseases for Oncology, version 3. | B-cell differentiation, pre-B-cells, B-precursor cells in lymphomas and leukemias | | 0‑L | 7 | 7 | International Classification of Diseases for Oncology, version 3. | Null-cell, non-B-nonT-cell differentiation in lymphomas and leukemias | | 0‑L | 8 | 8 | International Classification of Diseases for Oncology, version 3. | NK (natural killer)-cell differentiation in lymphomas and leukemias | | 0‑L | 9 | 9 | International Classification of Diseases for Oncology, version 3. | grading not applied, not applicable, unknown; cell type not assessed or unknown |
| | 0‑L | ASKU | Asked but unknown | Null Flavor | |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |
ICD-O-3 Topography 1.3.6.1.4.1.19376.1.3.11.36
| Id | 1.3.6.1.4.1.19376.1.3.11.36 | Effective Date | valid from 2015‑11‑13 19:16:23 |
|---|
| Status |  Draft Draft | Version Label | 1st rev. (2013) |
|---|
| Name | icd-o-3-topography | Display Name | ICD-O-3 Topography |
|---|
| Description | International classification of diseases / oncology, topographical part for typing of benign and malignant tumors. The topography axis (C-axis) uses the ICD-10 classification of malignant neoplasms (except those categories which relate to secondary neoplasms and to specified morphological types of tumours) for all types of tumours, thereby providing greater site detail for non-malignant tumours than is provided in ICD-10. In contrast to ICD-10, the ICD-O includes topography for sites of haematopoietic and reticuloendothelial tumors. |
|---|
A valid code from the code system:| Code System Name | Code System Id | Code System Version | | International Classification of Diseases for Oncology, version 3. | 2.16.840.1.113883.6.43.1 | |
|
| Or one of the following: |
| 2 Source Code Systems | 2.16.840.1.113883.6.43.1 - International Classification of Diseases for Oncology, version 3. 2.16.840.1.113883.5.1008 - Null Flavor |
|---|
| Level/ Type | Code | | Code System |
|---|
| | 0‑L | ASKU | asked but unknown | Null Flavor |
|
| Legenda: Type L=leaf, S=specializable, A=abstract, D=deprecated. NullFlavors to appear in @nullFlavor attribute instead of @code. |